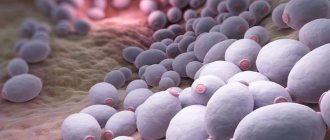
With the development of candidal vaginitis - vaginal thrush, the microflora is inevitably disrupted. The fungus of the genus Candida is an integral part of the female microflora, but when it actively multiplies, it disrupts it.
Normally, the main part of the flora is not Candida, but lactobacilli and bifidobacteria. To normalize the quantitative ratio of these microorganisms, gynecological specialists prescribe suppositories to patients to restore the microflora after treatment for thrush.
What is the best way to treat dysbiosis?
Most often, probiotics are used to restore beneficial microflora after thrush. They contain various bifidobacteria that are beneficial to the body.
Available in the form of solutions, drops, tablets and suppositories. Suppositories for restoring microflora after treatment of thrush are the most convenient form, as they are inserted directly into the vagina.
Vagilak
These suppositories contain calendula tincture to restore microflora. It has a healing effect and strengthens the immune system. Vagilak suppositories are used once a day at night after taking a shower. The standard course of therapy with these suppositories is 1–2 weeks, but this time may increase or decrease as prescribed by the doctor.
This drug for restoring balance has virtually no contraindications, however, during the course of treatment it is advisable to refrain from alcohol, smoking and sexual intercourse. Also, these suppositories should not be used during pregnancy.
Ecofemin
Herbal suppositories prescribed to restore microflora after treatment of thrush, made on the basis of field chamomile extract. This plant has a disinfecting effect, relieves burning and eliminates dryness in the intimate area. The therapeutic course lasts from 10 to 14 days. If a recurrence of thrush occurs, then to restore the balance, the time of use is reduced to a week. 2 candles are used per day - one in the morning and one in the evening.
Contraindications for use are diseases of the cardiovascular and nervous systems, as well as pregnancy. During the period of treatment with Ecofemin suppositories, gynecologists recommend giving up alcohol and smoking.
Often, in combination with Ecofemin, doctors prescribe chamomile tincture, which must be taken simultaneously with the introduction of suppositories on an empty stomach. The use of such a tincture will help to act more effectively on the body and quickly restore beneficial microflora after the end of treatment. This will also help reduce the risk of thrush recurrences.
Bifidumbacterin
This is a fairly well-known drug that is available in various forms. The main active ingredient is bifidobacteria, which restore the acidic environment in the vagina and, when actively multiplying, have a depressing effect on the Candida fungus.
Bifidumbacterin suppositories actively cleanse microflora and can be used to restore the balance of bacteria in the intestines.
The course of treatment with these suppositories is 10 days. It is necessary to administer 3-4 suppositories per day, depending on the state of the microflora. Restoring beneficial microorganisms with the help of these suppositories is possible even during pregnancy; they are usually prescribed after 8 weeks.
While restoring the balance of microorganisms, it is not advisable to use antipyretic drugs and antibiotics.
Vaginorm-S
These suppositories contain a large amount of ascorbic acid, which maintains the necessary acidity. In addition, the drug eliminates all microorganisms that irritate the uterine epithelium.
The therapeutic course is 10–14 days, 1 suppository is used daily. For more effective treatment, gynecologists recommend drinking as much water as possible throughout the course. Vaginorm-S is contraindicated in girls under 18 years of age and is not recommended for use in combination with antibiotics.
Lactobacterin
The medicine is made on the basis of lactobacilli acidophilus, and thanks to this it has a stimulating effect on the functioning of the immune system, improves metabolism and restores the balance of microflora. Lactobacterin suppositories to restore microflora after thrush must be used for 2 weeks, 3 suppositories per day. In addition, Lactobacterin is prescribed 10 days before birth and can be used during breastfeeding. Contraindication to the use of these suppositories is age under 18 years.
Pimafucin
These vaginal suppositories are made based on lactobacilli and lactic acid. Restore normal acidity and fight pathogenic microorganisms. Most often they are prescribed in combination with Vagikal drops. Suppositories are administered three times a day for two weeks.
The drug is compatible with antibiotics, but is not recommended for pregnant women and young girls. These suppositories cannot be used to restore microflora in some gynecological diseases and intestinal pathologies.
Application of traditional methods
Several folk methods are known to restore the vaginal microflora after thrush with beneficial microorganisms. A positive effect is achieved through the combined use of medications and folk remedies. The following methods are used:
- douching or sitz baths with decoctions of medicinal herbs - sage, chamomile, calendula;
- insertion of cotton swabs soaked in kefir or yogurt;
- tampons soaked in a solution of aloe juice and honey.
Such a popular method as douching with a soda solution has proven itself well. To carry out the procedure, you need to dissolve 5 g of baking soda in 1 liter of boiled warm water. The proportions cannot be exceeded, as soda can harm dry and damaged mucous membranes.
You should reconsider your diet. A woman during thrush and during the period of recovery of the body should not drink alcohol, fatty meat, baked goods made from yeast dough, or a lot of sweets.
Recommendations for establishing microflora
Disturbance of the microflora after candidiasis is otherwise called vaginal dysbiosis. Your own feelings will help you determine the presence of this problem. In most cases, women experience itching in the vagina. However, such symptoms occur only during the exacerbation of the disease. If the disease is in its early stages, then it may not have pronounced symptoms. Therefore, in order not to miss the development of the problem, it is recommended to visit a doctor after treating thrush. The doctor will conduct the necessary examination and make a diagnosis.
It is known that a healthy vaginal microflora involves the presence of 90% lactobacilli, 9% bifidobacteria and 1% opportunistic microorganisms. Based on this, restoring it does not mean completely destroying the fungus.
The main task is to achieve the required ratio of these indicators, that is, a balance between beneficial and harmful vaginal bacteria is required. Microflora can be restored artificially:
- The doctor prescribes medications that help relieve discomfort.
- Thanks to their effects, beneficial bacteria multiply and healing of the vaginal mucosa occurs.
An important condition for resuming the normal functioning of the female genital organs is the establishment of the functioning of the immune system. If this is not done, a relapse of the disease may occur. In addition, you should be treated together with your sexual partner. By neglecting this rule, a woman can become infected with thrush again.
Another important point is the restoration of the superficial vaginal epithelium damaged by infection. In order for prebiotic agents to adhere well to the walls of the damaged organ and have a therapeutic effect, the upper layers of the epithelium must be healthy.
Restoring the vaginal microflora includes several mandatory steps. The first step, using antifungal medications, is to suppress and destroy the Candida fungus, which is a pathogenic microorganism
Next, it is important to reconstruct the vaginal epithelium. The next condition is to restore the number of beneficial microorganisms
In addition, the doctor will necessarily prescribe immunomodulatory drugs that allow the immune system to function normally.
Despite the apparent simplicity of resolving the problem, you should not self-medicate. After all, each human body is individual, and therefore requires a special approach. Before prescribing treatment for dysbiosis, the gynecologist will determine the stage of development of the disease and determine the possibility of the presence of concomitant diseases. The patient’s age, his body’s tendency to allergic reactions and other circumstances must be taken into account.
Prevention measures
Restoring the microflora of intimate areas is not so easy, so it is better to follow preventive measures that will prevent the disease from developing. It is important to follow a diet not only during treatment, but also every day in order to prevent any diseases, including dysbacteriosis.
It is important to maintain the normal functioning of the immune system by consuming a complex of vitamins and maintaining personal hygiene. Stressful situations should be avoided whenever possible.
Thus, it is possible to restore healthy vaginal flora with the help of medical and folk remedies. However, this process can take quite a long time. In order not to cause even more harm to your health, you must promptly seek qualified help.
Symptoms of thrush
Vaginal fungus (dysbacteriosis, thrush, candidiasis) is an infectious disease of the female reproductive system that can spread to the uterus and labia.
Pathology develops due to the growth of colonies of the Candida albicans family. The conditionally pathogenic part of the microflora becomes active under the influence of certain factors. The disease cannot be ignored, otherwise it will develop into colpitis, cystitis or urethritis.
The predisposition to vaginal mycosis is influenced by a number of factors:
- Weak immunity.
- Frequent stress.
- Hypothermia.
- Tuberculosis.
- Immunodeficiency.
- Beginning of sexual activity.
- Intestinal dysbiosis.
- Venereal disease.
- Failure to maintain intimate hygiene.
- Promiscuous sex life.
- Unprotected sex.
- General intoxication of the body.
- Abuse of douching.
- Physical or mental fatigue.
- Severe infectious diseases.
- Microtraumas on the vaginal mucosa.
- Wearing tight underwear made of synthetic materials.
- Endocrine disorders (hypothyroidism, diabetes mellitus, changes in hormonal levels due to pregnancy and taking hormonal contraceptives).
- Long-term use of systemic and external antibiotics.
- Poor nutrition and addiction to bad habits.
The risk of urogenital candidiasis increases for women at the end of menstruation. It is easier for fungus to develop if a woman has poor personal hygiene - she rarely washes or walks for a long time with one pad. Untimely change of panty liners is also fraught with vaginal dysbiosis.
The disease is manifested by curdled vaginal discharge, itching, burning and redness of the mucous membrane. The fungus spreads to the skin of the perineum and anus.
In severe cases, the fungus grows and appears in the mouth, on the skin and under the nails. Then the gastrointestinal tract is affected. Loose stools mixed with white flakes appear.
Dysbacteriosis has specific symptoms that are well studied. The main symptoms of bacterial vaginosis:
- abundant mucous discharge of a whitish (sometimes yellow or grayish) hue, which has a specific unpleasant odor;
- burning, itching of the external genitalia, symptoms worsen during sexual intercourse, during menstruation;
- nagging pain in the lower abdomen;
- dryness of the external genitalia;
- pastiness of the external genitalia, becoming bluish-red;
- painful sensations, discomfort during sexual intercourse, which appear at the beginning or last throughout intercourse and intensify at the end;
- other symptoms that depend on the type of pathogen, for example, if the growth of candida predominates, curdled discharge appears, if gardnerella smells like rotten fish.
Symptoms of the disease
The main manifestation of thrush in the intestines will be severe pain, in addition to which you should pay attention to the following signs of invasion:
- bloating becomes chronic;
- patients complain of heaviness in the epigastric region (stomach);
- after eating, intestinal spasms are observed;
- impaired intestinal motor function (diarrhea);
- low-grade body temperature (from 37 to 37.5 0);
- patients complain of lack of appetite;
- impurities of blood and pus are found in the stool;
- in the anal area and stool you can find a cheesy discharge with a foul odor;
- after bowel movement there is no feeling of relief;
- pain during defecation;
- false urge to defecate;
- a rash appears on the skin.
In addition to the primary signs of pathology, fatigue, insomnia and various forms of skin diseases (acne, dermatitis, urticaria) may appear.
Regardless of the severity of the clinical picture, intestinal candidiasis can be easily determined by an experienced doctor (gastroenterologist).
As the pathological spread of fungi progresses, all symptoms intensify. Lack of treatment allows the pathology to spread to various parts, most often the disease affects the genitourinary organs and the oral cavity. In addition to spreading, candidiasis provokes an exacerbation of existing diseases of the gastrointestinal tract.
The transition of thrush from the intestines to the genitals in a woman has the following symptoms:
- cheesy discharge is detected on the genitals and underwear, having an unpleasant odor;
- unbearable itching of the vagina, turning into a burning sensation, can be observed at rest, during urination or sexual intercourse;
- in severe forms of the disease, menstrual function may be impaired; long-term infection can cause secondary infertility.
Symptoms in men are not very different:
- itching and burning of the penis and scrotum;
- discharge of a cheesy nature (outwardly reminiscent of cottage cheese);
- disturbance of urination, pathogenic fungi are detected in the urine (visually the urine has a cloudy whitish sediment).
When the oral cavity is affected, inflammation of the mucous membrane, a white coating that can be easily removed with a spatula or gauze swab, and pain during eating are determined.
Medications
After treatment for thrush, many women complain of excessive vaginal dryness, the main cause of which is medications. How to restore flora after thrush? Which drugs should be preferred? You can find the answers to these questions in the following table.
| Medicines to be used after treating thrush | |
| Ecofemin | Helps lactobacilli convert excess glycogen secreted by the vaginal mucosa into lactic acid. Excellent healing of all wounds and microcracks that formed during thrush. The course of treatment with this remedy is designed for 10 days. |
| Vagilak | It allows not only to populate the microflora with beneficial microorganisms, but also to create ideal conditions for their development. The duration of taking the drug and the intensity of its use must be agreed with the attending physician. |
| Femilex | At their core, these suppositories that restore microflora are a concentrate of lactic acid, without which the proliferation of lacto- and bifidobacteria is impossible. The course of treatment can last from a week to 10 days. |
| Vagical | It perfectly heals all wounds and other damage to the mucous membrane, since it contains calendula extract, a plant that has long been famous for its healing properties. It also allows you to normalize the secretory function. |
| Acylact | These suppositories simultaneously restore the acid balance of the vagina and fight pathogenic microorganisms due to acidophilic beneficial bacteria that are part of the drug. |
| Lactobacterin | The drug contains lactobacilli, which will help normalize the vaginal microflora, as well as stabilize its acid-base balance. The full course lasts 10 days, during which this product must be used twice a day. At the end of taking it, you should definitely do an analysis of the state of the flora. |
Drugs should be selected by the attending physician strictly individually. The prescription of a particular drug depends on the form of the disease, complications, the presence of other infections, the dynamics of the development of pathogenic microorganisms, and the state of the microflora.
Special vaginal probiotics, which contain lactobacilli, perfectly restore microflora - they can be produced in tablets and in the form of suppositories
It is important not to make a mistake with the choice of drugs: any inflammation or infection destroys the upper layer of the epithelium, and it seems to slough off
After treatment of thrush and the disappearance of the clinical symptoms of the disease, doctors recommend treatment with vaginal tablets Vaginorma S. The drug restores normal acidity of the vagina, and thereby stimulates the reproduction and growth of beneficial bacteria. Additionally, suppositories are prescribed - they will restore beneficial microorganisms of the flora. Medicines Bifidumbacterin and Lactobacterin are prescribed by specialists to be taken in a course - for 10 days.
The drug Gynoflor, available in the form of vaginal tablets, is widespread; Ecofemin and Vagilac are no less popular among specialists.
Another effective remedy for restoring vaginal microflora is Kipferon suppositories. Treatment with this drug takes place in courses: to completely restore the microflora, you need to take 2-3 courses with a week break.
A specialist may prescribe the drug Normoflorin-B or Normoflorin-L. It is recommended to take these remedies twice a day, morning and evening, for a month.
Intimate protectors - Doderlein sticks
The vaginal microbiocenosis contains Doderlein bacilli. The cleanliness of the female vagina is determined by the quantitative ratio of these microorganisms and cocci. A significant decrease in the level of the first bacteria leads to the development of vaginal bacteriosis. Thus, Doderlein's bacilli perform a protective function, which is to maintain an acidic environment.
These bacteria produce immune cells that actively fight pathogenic microorganisms. If a woman’s body produces an insufficient number of Doderlein bacilli, it means that pathological processes are occurring in the reproductive system. In this case, gynecologists prescribe an additional test - bacterial culture - to determine the reason for the decrease in the level of these beneficial bacteria.
Candles "Vaginorm S"
Vaginorm S suppositories support vaginal acid
Release form: candles. The drug contains a large amount of ascorbic acid. Maintains the acidic environment of the vagina. Eliminates bacteria and viruses that cause irritation of the uterine epithelium. Has an antiseptic effect.
The course of treatment involves 10 or 14 days according to the individual indicator. Use 1 suppository per day. To obtain effective results, gynecologists recommend drinking more water.
In case of relapse, the period of use is 2-3 months. The drug is contraindicated in underage girls. Allowed in the 1st semester of pregnancy. Special instructions: do not use with antibiotics.
Medicines
It is important to receive complete treatment in several stages from a gynecologist with mandatory control smears both at the beginning and at the end of therapy
4.1. Clindamycin
This is a broad-spectrum antibiotic that successfully works against opportunistic and pathogenic vaginal flora.
It allows you to significantly reduce its quantity and gives beneficial lactobacilli a chance to multiply. Contraindicated in the first trimester of pregnancy.
It has different trade names in the pharmacy chain and is available in the form:
- 1 candles – Klindacin, Dalatsin.
- 2 Kremov – Clindamycin, Dalatsin, Clindacin Prolong.
- 3 capsules for oral administration and solution for intramuscular administration.
4.2. Metronidazole
It is active not only against pathogens, but also against protozoa, for example, Trichomonas.
Contraindicated in the first trimester of pregnancy and while breastfeeding. List of release forms for the treatment of bacterial vaginosis:
- 1Suppositories – Mistol, Flagyl, Metronidazole, Metrovagin.
- 2Vaginal tablets – Trichopolum.
- 3Vaginal gels – Metrogyl.
- 4Tablets and capsules for oral administration – Metronidazole, Klion, etc.
- 5Combined drugs - Vagisept suppositories (metronidazole + fluconazole), Vagiferon (with the addition of interferons), Metromicon-Neo, Neo-Penotran (metronidazole + miconazole), vaginal tablets Klion-D (metronidazole + miconazole).
4.3. McMirror
Nifurantel actively destroys bacteria, protozoa and fungi. In combination with nystatin, which has an antifungal effect, its effectiveness increases even more.
In the pharmacy chain, the combination of nifurantel and nystatin is known as Macmiror Complex (these are soft vaginal capsules). The drug is widely used at the first stage of normalization of microflora. Contraindicated in the first trimester of pregnancy.
4.4. Terzhinan
These are vaginal tablets containing ternidazole, neomycin, nystatin and prednisolone.
Ternidazole and neomycin successfully destroy Gardnerella and other microorganisms that predominate in dysbiosis.
Thus, the drug changes the ratio in favor of beneficial lacto- and bifidobacteria. Nystatin has an effect on yeast fungi, and prednisolone eliminates the inflammatory response.
Terzhinan is indicated at the first stage of restoration of microflora in cases of bakvaginosis and vaginitis.
4.5. Antiseptics
When applied topically, it is practically not absorbed into the blood and does not have a systemic effect.
For use in gynecology, chlorhexidine is available in the form of suppositories (Hexicon, Hexicon D) and combination preparations (Depantol suppositories - dexpanthenol + chlorhexidine), which can be used for treatment during pregnancy and lactation.
Dequalinium chloride (the main active ingredient of the drug) is an antiseptic that is active against most gram-positive and gram-negative bacteria, fungi of the genus Candida and Trichomonas.
It is also used in the first stage of restoring the vaginal microflora. Povidone-iodine is often prescribed to prevent candidiasis.
The most common forms of release used in gynecology are Betadine and Iodoxide suppositories.
4.6. Clotrimazole
It has different release forms, of which the most often prescribed in gynecology are:
- 1Vaginal tablets – Candibene, Canesten, Clotrimazole.
- 2Gels, vaginal creams – Candide, Clofan.
- 3Combined suppositories – Vagiclin (clotrimazole + clindamycin), Clomegel (metronidazole + clotrimazole).
4.7. Natamycin
This is a natural antibiotic that has a detrimental effect on pathogenic fungi, including candida.
Its distinctive feature is the almost complete absence of allergic reactions. Can be used during pregnancy and breastfeeding.
In gynecology, its dosage forms are used in the form of pessaries (Natamycin) and vaginal suppositories (Pimafucin, Pimafungin).
4.8. Econazole
Contraindicated in the first trimester of pregnancy. Release forms - creams and suppositories (Gyno-Pevaril, Ekalin, Econazole, Ifenek).
Special therapy
If therapy is not organized correctly, only one partner is treated for thrush - there will be no effect. If prescribed medications that restore the flora damaged by pathogenic microorganisms and the upper layer of the vaginal epithelium are not taken, then treatment with even the most modern probiotics will either have a short-term effect or not have it at all.
Special therapy to restore vaginal flora includes the following steps:
- suppression of pathogenic microorganisms;
- restoration of bacteria necessary for the body;
- regulation of the immunity of the vaginal walls.
In this regard, an experienced specialist prescribes medications with different effects:
- antifungal pharmacological drugs;
- probiotics with lactobacilli and bifidobacteria;
- as well as drugs that restore immunity: local immunomodulators and general ones.
How to restore vaginal microflora after thrush?
The causes of disturbed microflora are considered:
- presence of chronic diseases;
- long-term antibiotic therapy;
- decreased immunity;
- reduced body resistance;
- hormonal imbalances;
- menopause;
- unbalanced diet;
- sudden climate change.
During a long course of antibiotics, not only pathogenic bacteria, viruses and fungi are destroyed, but also healthy cells of the body. Excellent conditions are created for the growth of Candida fungus. The risk of new diseases emerging against the background of decreased body resistance increases.
Before restoring the flora, it is necessary to increase the body’s immunity, identify the cause that caused candidiasis and eliminate it.
The etiology of pathological reproduction of candida in the oral cavity is not much different from the standard:
- pregnancy;
- hormonal imbalances;
- decreased immunity;
- taking hormonal drugs, antibiotics;
- avitaminosis;
- oral contraceptives;
- smoking;
- injuries to the oral mucosa, complicated by the ingress of secondary microflora;
- chemotherapy and radiation therapy;
- dentures.
Infants become infected with candidiasis during childbirth, provided that the mother in labor has the disease.
- immaturity of the oral mucosa;
- feature of immunity;
- prematurity;
- microflora instability;
- violation of the removal of acids from the body.
Vaginal lesions
The etiology of vaginal candidiasis may be:
- wearing uncomfortable underwear;
- poor or improper intimate hygiene;
- diabetes;
- chronic diseases;
- decreased immunity;
- antibiotic therapy;
- chronic diseases.
In men, this disease occurs for the following reasons:
- after sexual intercourse
- due to stress;
- overwork;
- carbohydrate diet;
- dysbacteriosis;
- trauma to the penile mucosa.
Oral and nasal cavity
The yeast fungus Candida, which causes thrush, multiplies well in the mouth, disrupting the normal microflora of not only the oral cavity, but also the nose. Dysbacteriosis of the oral cavity and nose is manifested by drying out of the mucous membranes, the appearance of microcracks on them, difficulty in nasal breathing, and the formation of bloody crusts in the nose. The same symptoms are observed after long-term use of antibiotics or after a course of systemic antibiotics - by the way, it is often antibiotics that disrupt the normal bacterial balance in the body and provoke the pathological proliferation of Candida fungi.
You can also restore the microflora of the mouth and nose by taking and topical application of probiotics (there are special preparations in drops that can be instilled directly into the nasal sinuses). It is also important to exclude from the diet foods that affect the bacterial background and the proliferation of fungi - the list of products is the same as in the case of gastrointestinal dysbiosis.
Probiotics in the form of nasal drops help well during the rehabilitation period