The ovaries in the female body are the basis of its ability to conceive a child. Their constant activity in the form of maturation, descent through the fallopian tubes into the uterus and excretion of eggs after fertilization has not occurred, ensures the menstrual cycle. This also explains the fluctuations in hormonal levels that are observed naturally in women until menopause.
The ovaries constantly produce estrogen hormones, which form the female background. But they can also get sick both for reasons that cause any organs of the body to get sick (injuries, infections), and because of their own “disagreements” with other organs that synthesize sex hormones. For example, in addition to the main glands (in men these are the testes), both sexes also have the adrenal cortex in their bodies - the producer of many corticosteroids, including hormones of the opposite sex.
Testosterone serves the female body in the same capacity as estrogen serves the male body. Namely, as an estrogen antagonist, a stimulator of ovarian activity. When testosterone levels rise, they respond by increasing their activity. In addition, the presence of “opposite” hormones allows us not to turn into asexual creatures after menopause.
However, if during puberty the balance of these two scales is disturbed, the consequences are reflected primarily on them. That is why problems with procreation are among the most stubborn to all attempts to cure them.
What is ovarian resection in women?
Ovarian resection is a surgical procedure in which the tissue of the reproductive gland is partially removed. To do this, several punctures are made in the abdominal wall. Although previously the operation was performed through an incision in the abdomen.
During surgical procedures, the doctor must excise the affected part of the ovarian tissue. But the gonads are not completely removed. In polycystic disease, surgery is needed to facilitate the release of the egg from the follicles. After all, with the disease, the capsule of the gonads thickens, and the oocyte cannot break through this membrane. In place of the follicles that did not burst, multiple cysts appear. Over time, in the absence of treatment, the situation only gets worse.
When performing a wedge resection, part of the ovary is cut out in the form of an acute triangle. Thanks to this type of operation, it is possible to eliminate the associated factors of infertility. The likelihood of pregnancy after surgical procedures increases by 70-80%.
Clinical manifestations
Clinical manifestations of ovarian cancer during pregnancy are usually absent. The diagnosis is made by incidental finding on ultrasound, during cesarean section, or by clinical manifestation of the disease in the postpartum period [4]. According to the results of a retrospective study of 8330 cesarean sections, 68 cases of newly diagnosed ovarian tumors with a diameter of more than 5 cm were described, and only 1 of them was confirmed to be malignant [8].
Nonspecific symptoms of OC include abdominal and back pain, constipation, bloating and dysuria [9, 10]. Acute pain may be associated with partial or complete torsion of the adnexa, which occurs in 5% of pregnant women. When the size of the formation is from 6 to 8 cm, the probability of torsion reaches 22%, 60% occurs in the interval from 10 to 17 weeks. pregnancy. After 20 weeks pregnancy, the probability of torsion does not exceed 6% [3, 11].
Indications and contraindications for the procedure
Most often, resection is prescribed for patients diagnosed with polycystic disease. But surgical intervention is indicated in cases where conservative therapy is ineffective.
Resection can also be performed if:
- ovarian apoplexy;
- cystic formations;
- benign tumors;
- foci of endometriosis;
- purulent inflammation of the appendages;
- rupture of the cyst or torsion of its stem;
- ectopic pregnancy attached in the area of the appendages.
All cystic formations, tumors, and ectopic pregnancies are removed in such a way as to preserve the ovarian tissue as much as possible. In polycystic disease, the surgeon cuts out overgrown tissue. In some cases, it can remove 2/3 of the volume of the gonad.
Surgery is not recommended for women who:
- exacerbation of infectious and inflammatory diseases of the genitourinary system;
- fever;
- disruption of the blood coagulation system.
Once the condition has returned to normal, a date for resection can be set. Ovarian tissue should not be excised if there is a suspicion that the tumors on them are malignant.
Ovarian resection methods
Before performing surgery, the surgeon must tell the patient which surgical method will be used. Depending on the situation, a unilateral resection is performed or the tissue of two ovaries is excised.
Reference! With polycystic disease, doctors operate on both sex glands at the same time.
The doctor can perform resection using laparoscopic or laparotomy access. The choice of method depends on the equipment located in the clinic and the woman’s health condition.
Laparotomy resection of the ovary
Laparotomy is performed on patients if urgent surgery is required. It is carried out when:
- ovarian apoplexy;
- rupture of the cyst or twisting of its legs;
- emergency condition arising from a diagnosed ovarian pregnancy.
Planned laparotomy in modern clinics is performed only on those patients who have a pronounced adhesive process in the pelvic area. Laparoscopy is contraindicated in this situation.
During laparotomy, the surgeon makes an incision from top to bottom along the midline of the abdomen or in the suprapubic region in the transverse direction. Through the incision, he gains access to the appendages, can examine them, remove identified adhesions, isolate the gonad and operate on it.
Laparoscopic ovarian resection
Most elective pelvic surgeries are performed laparoscopically. This type of access has many advantages:
- minor tissue trauma;
- reduction of the recovery period;
- reducing the period of incapacity.
Attention! Thanks to the organization of laparoscopic access, it is possible to reduce the likelihood of developing postoperative complications. Adhesions in the pelvic area after laparoscopy occur much less frequently than after laparotomy.
During laparoscopy, 3-4 punctures are made in the patient’s abdominal wall, through one of them the cavity is pumped with gas to move the organs away from the abdominal walls and from each other. This allows you to conduct a full examination and determine the required volume of surgical intervention.
A laparoscope is inserted into the abdominal cavity through a puncture. This is a special endoscopic instrument equipped with a video camera and a light source. Surgical instruments are inserted through other openings. The parenchyma of the gonad is dissected with an electrocoagulator using high-frequency electric current. A high temperature is created in the area of its action, thanks to which small vessels are sealed, the risk of postoperative bleeding is minimized.
Technique of wedge resection of the ovary
If it is necessary to perform a resection, the gynecologist, having gained access to the ovary, compresses the pedicle of the gonad, in which the arteries pass. After this, the ovarian tissue is excised in the shape of a wedge, the tip of which is directed inward.
It is important to cut out part of the ovary so as not to disrupt blood circulation in this organ. The doctor must remove a minimum amount of ovarian tissue, cut out sclerotic formations and the immature follicles remaining in them.
After removing the desired fragment, the ovary is sutured with self-absorbing threads using thin needles. All manipulations must be done so that thin tissues are not injured. All bleeding vessels are bandaged.
Oncological prognosis
Oncological prognosis in pregnant women with ovarian cancer was presented by Norwegian researchers N. Stensheim et al. (2009) [35]. There was no significant association between pregnancy and mortality from ovarian cancer, but this risk increased in breastfeeding women (HR 2.23; 95% CI, 1.05–4.73; p=0.036). A study that included 105 pregnant women with ovarian cancer showed that the worst prognosis was for poorly differentiated tumors and advanced stages of the disease; the 2-year survival rate of such patients was 30.0% and 25.0% (stage IV), respectively.
The literature contains 2 reviews (n=46 and n=102) devoted to nonepithelial ovarian malignancies and pregnancy [36]. The vast majority of patients (>76%) were diagnosed with stage I disease and had a favorable oncological prognosis. In patients with sex cord stromal tumors, pregnancy was maintained in 69.4% of cases [36]. Of these, 13% required chemotherapy, but only 4% received it during pregnancy. The overall 5-year survival rate was 89.3%. With advanced tumor processes (stages II–IV), survival was significantly lower (5-year survival rate for stages II–IV was 70% versus 100% for stage I, p=0.008). Relapses and rapid progression of the disease in sex cord stromal tumors occurred in 8.7% and 2.2% of cases, respectively. The second report concerns pregnant women with ovarian germ cell tumors (n=102), the majority of which were unilateral (84.3%) and diagnosed at an early stage (76.4%) [37–39]. More than half of the patients (52.0%) received systemic chemotherapy using the regimen of cisplatin with bleomycin. In 7 (6.9%) patients, relapse occurred during pregnancy. Alpha-fetoprotein was elevated in only 4 (57.1%) patients with relapses of the disease, which once again emphasizes the limited possibilities of its use in monitoring pregnant women suffering from this pathology. Most often, recurrent tumors in pregnant women were localized in the abdominal cavity. The overall 5-year survival rate was 80.1%. Young patient age (≤20 vs. >20), large tumor size (<20 cm vs. ≥20 cm), and advanced stage of disease (II–IV vs. I stage) are the most important prognostic factors associated with poor prognosis. At the same time, the stage of the disease remains an independent prognostic factor (HR 21.6, 95% CI 2.06–226, p=0.01).
Types of surgery
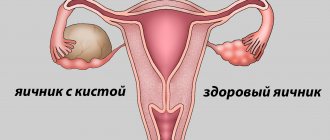
Depending on the established diagnosis, the condition of the gonads and the goals set, the doctor selects the type of operation. In case of polycystic disease, resection of both ovaries is performed. If cystic formations are detected on one side, resection of the right or left ovary may be prescribed. In some cases, partial resection is sufficient. But there are situations when it is necessary to completely remove the gonad or all appendages.
Partial resection
In women of reproductive age, if possible, only partial resection is performed. This operation is less traumatic, and it is possible to preserve reproductive function.
This method is mainly used to identify single cysts, polycystic disease, inflammatory changes in tissues, ruptures, and torsion of cysts. After the operation, after some time, the operated organ is completely restored and begins to perform its functions again.
Resection of the left ovary
Removal of tissue from the left gonad is necessary if there are formations on it that need to be removed. The left ovaries in most women are smaller than the right ones, and they have fewer follicles. Therefore, the likelihood of impaired reproductive function during operations on them is lower than during resection of the right gonad.
Resection of the right ovary
According to statistics, resection of the right gonads is performed more often. This is due to the fact that many patients have better blood circulation on the right side, so problems on this side arise more often.
If a large cyst, tumor, or ectopic pregnancy is detected on the right ovary, the doctor can cut out part of its tissue. The probability of maintaining reproductive health after such work by surgeons reaches 70%.
Resection of both ovaries
Most often, surgery on both sex glands is performed on patients diagnosed with polycystic disease, which is not amenable to drug therapy. After all, sclerotic tissue must be removed from both sides. This will increase the chances of ovulation and pregnancy.
Bilateral resection is performed both for polycystic disease and for detection of bilateral pseudomucinous or endometrioid cysts.
Chemotherapy
After surgical staging, chemotherapy is indicated for all pregnant women with ovarian cancer. The exception is patients with stage IA ovarian cancer (G1, G2). In cases of advanced ovarian cancer, chemotherapy may be the only treatment option to maintain pregnancy [27].
At the same time, treatment regimens for pregnant women should not differ from those for non-pregnant women with this pathology. Chemotherapy is contraindicated in the first trimester of pregnancy, since its administration can lead to termination of pregnancy, intrauterine fetal death, as well as to malformations [27]. In the second and third trimesters, chemotherapy can cause fetal growth restriction, prematurity, low birth weight, and stillbirth [28]. The side effects of chemotherapy on the mother's body are the same as in non-pregnant women receiving chemotherapy, i.e., they can manifest as myelosuppression, in particular neutropenia. Pregnant women are prescribed a standard chemotherapy regimen for ovarian cancer: paclitaxel with carboplatin. Studies conducted in animal models have shown that taxanes do not affect organogenesis and cognitive function. However, the penetration ability of these drugs across the transplacental barrier in humans is not fully known [29–31].
Non-epithelial neoplasms of the ovaries (germ tumors, as well as sex cord stromal tumors) in pregnant women are diagnosed, as a rule, at stage I; the main method of their treatment is removal of the affected uterine appendages while preserving the contralateral ovary. If the contralateral ovary is visually unchanged, it is not advisable to perform a biopsy. For sex cord stromal tumors, postoperative chemotherapy is indicated for patients starting from stage IC. In patients with malignant germ cell tumors after surgery, chemotherapy is not indicated for stage IA GI immature teratoma or stage IA dysgerminoma. In advanced stages, adjuvant chemotherapy is indicated, the same as for non-pregnant women. For them, the standard regimen is a combination of platinum with etoposide (BEP or EP) [32]. Based on literature data, the main treatment regimen includes a combination of cisplatin (75 mg/m2) with weekly administration of paclitaxel (80 mg/m2) from the second trimester [32–34].
Rehabilitation
The recovery period after laparoscopy is much shorter. Patients recover in 2 weeks; after laparotomy, the rehabilitation period extends to 2 months.
When performing laparoscopy, the patient is recommended to start walking and perform simple movements in the evening of the operating day. This is necessary to prevent the occurrence of complications in the form of adhesions, thrombosis, and intestinal dysfunction.
You can prevent the occurrence of negative consequences after ovarian resection if you continue to follow the doctor’s recommendations after discharge:
- refuse sexual intercourse for 2-4 weeks;
- do not lift more than 3 kg;
- exclude herbs, spices, smoked food, and alcohol from the menu.
Medications are often prescribed to help prevent the pathology from returning. For many, the menstrual cycle recovers on its own after surgery.
Preparation
Even the slightest surgical intervention requires a preliminary examination to exclude possible complications, as well as to identify contraindications.
Naturally, before resection the patient will also have to undergo laboratory and instrumental diagnostic tests.
These include:
- Submission of biomaterials for analysis (blood to determine the indicators of formed elements, coagulability, group and Rh factor, hormone levels, the presence of signs of infectious diseases, urine, feces);
- Taking smears from the vagina to assess microflora;
- Conducting electrocardiography , fluorography, ultrasound, computed tomography if necessary.
In the preparatory period, the patient needs to follow a diet based on the consumption of foods that are not difficult for the food system to process. That is, you should not load the gastrointestinal tract with fatty, fried, smoked foods, high-calorie and rough foods that cause increased gas formation.
At least a week before the scheduled date, it is recommended to stop using medications, the effect of which may negatively affect the course of the operation. To do this, you should first consult with a doctor to decide which medications you can continue taking and which ones you can stop.
The day before the resection, the patient should minimally limit her food intake, and even water a few hours before the intervention. The preoperative stage also consists of studying the patient’s allergy history. If she has an allergic reaction to any drugs used during the operation, she needs to look for an alternative. An important hygienic point is the removal of hair from the pubic area. Colon cleansing is also performed using an enema.
Note! Following all the doctor’s recommendations during preparation will protect you from complications, because failure to comply with even the slightest rules of hygiene, when it comes to manipulations performed by surgeons in the human body, can lead to extremely undesirable consequences.
Why is part of the ovary left during surgery?
In the absence of indications for oophorectomy (complete removal of the ovaries), their tissue is only partially excised. This is necessary so that the sex hormonal glands can continue to work. Otherwise, irreversible changes begin in the female body.
The ovaries are a source of estrogens; a woman needs these hormones to maintain a normal physical and emotional state. When the gonads are removed, changes in the body begin that are similar to menopause. The difference is that the process of fading of their function in women after 45 years is gradual. And after the operation, hormones suddenly stop being produced, as a result the body experiences enormous stress.
Important! Partial preservation of the ovarian tissue in which the follicles are located helps the body continue to function as usual.
Is the ovary restored after resection?
When ovarian tissue is excised, its volume decreases. During the operation, the surgeon cuts out part of the follicles. Their number is formed in girls in utero, so there is no hope for complete restoration of the ovary after resection. Some people experience a process of stromal proliferation, but this does not affect reproductive function.
The decisive factor is not the size of the remaining part of the gonad, but the follicular reserve located in it. An approximate assessment of the condition of the gonad after surgery can be made by measuring its volume.
How long do the ovaries last after resection?
It is impossible to predict how long the reproductive glands will function after resection. Situations are possible when a woman calmly gives birth to several children and waits until menopause after 40 years, even if she had a resection at the age of 17. In some patients, the gonads may immediately refuse to function after surgery. As a result, the woman experiences an unplanned early menopause.
The duration of their work will depend on what part of the gland was cut out and how many follicles were removed. With a small follicular reserve remaining, doctors often prescribe hormonal drugs to patients; they are needed to delay menopause.
Obstetric prognosis
Pregnancy complicated by cancer always carries a high risk of complications, regardless of treatment methods. Prematurity, fetal growth restriction, and miscarriage (including stillbirth) are the most common obstetric complications. A population-based study conducted from 1973 to 2012 showed that cancer diagnosed during pregnancy was associated with high neonatal mortality, mainly due to fetal growth restriction and iatrogenic preterm birth [37]. In case of ovarian cancer and pregnancy, obstetric complications can be caused not only by the underlying disease, but also by complications resulting from surgical treatment and chemotherapy. A review published in 2015 described 105 cases of invasive ovarian cancer during pregnancy. The majority of pregnancies (81.3%) resulted in live births. The most common cause of fetal and newborn death was premature birth. In more than half of the patients (71.6%), delivery was performed by cesarean section. In women who received chemotherapy during pregnancy, no fetal malformations were identified, in addition, there was no statistically significant difference in fetal growth retardation during chemotherapy. Obstetric outcome in OC mainly depends on the stage of the disease and histological type of tumor.
What complications can there be?
After any surgical procedure, patients may experience the following problems:
- damage to abdominal organs;
- the occurrence of adhesions;
- development of bleeding;
- wound infection;
- allergy to drugs used in anesthesia.
Among the long-term complications of resection is the appearance of infertility. Therefore, a woman is recommended to start planning a pregnancy 1-2 months after the operation or is prescribed hormonal drugs that can help preserve the remaining follicles. Infertility can be caused by the development of adhesions in the pelvis, a decrease in the supply of eggs, and a deterioration in the production of sex hormones.
Recovery period
The most important days are the first. The more correctly doctors provide medical care and prescribe treatment, the more successful the result will be.
You are allowed to get out of bed on the second day. A special place here is occupied by the hygiene of postoperative wounds. Nurses are required to change gauze bandages every day and treat stitches with a special solution.
It is believed that the woman will fully recover in a month. Sexual rest must be observed for two weeks; you can play sports after 30 days. It is also recommended not to take a bath for 10 days.