Non-lactation mastitis is a disease in which an inflammatory process occurs in the mammary gland. Unlike lactation mastitis, it has nothing to do with breastfeeding. That is why this pathology can develop in patients of absolutely any age.
Non-lactation mastitis is a common disease that is diagnosed in patients of all ages.
Important! Most often, women who experience hormonal changes in their bodies experience non-lactation mastitis.
Why does mastitis occur?
The main cause of the development of the disease is considered to be hormonal disorders. Non-lactation mastitis occurs in women during menopause, when estrogen levels drop, and in girls of puberty. Symptoms of this disease are not excluded even in young children.
Certain factors can also provoke mastitis in non-breastfeeding women:
- mechanical damage and injury to glandular tissue if infection gets into the wound;
- weakened immunity due to certain diseases (diabetes mellitus, vitamin deficiency);
- operations on the mammary gland.
In infants, mastitis is usually diagnosed in the first weeks of life. The mammary glands swell and secretion accumulates in them, which cannot be squeezed out. The main cause of non-lactation mastitis in young children is hormonal imbalance. The disease does not require treatment and goes away on its own in about a month.
Causes
The most common causes of non-lactation mastitis include:
- excess estrogen and progesterone;
- decreased immunity;
- surgical intervention on the mammary gland;
- the presence of foci of infection in the body;
- severe single chest injuries or minor but permanent ones;
- hypothermia of the body;
- wearing the wrong bra;
- swimming in ponds with dirty water;
- deficiency of vitamins and minerals.
Mastitis can occur due to severe hypothermia
Important! Non-lactation mastitis never affects both mammary glands at once.
Signs of non-lactation mastitis
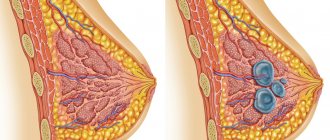
The development of the pathological process begins with inflammation of the mammary glands. Initially, the symptoms of mastitis in non-breastfeeding women are mild. Then the secretion of the mammary glands increases, minor discomfort and swelling appear. At the site of inflammation, the skin sometimes darkens and retracts. Such symptoms force a woman to see a doctor. At this stage, the disease is highly treatable.
Breast mastitis in non-lactating women has several development options. Therefore, it is advisable to consider the clinical picture of the disease in relation to each form of the disease.
How to treat mastitis in non-breastfeeding women
Can a woman who is not breastfeeding have mastitis? Why does this disease occur, how to prevent it, what are the prevention and treatment measures? Many are sure that this misfortune occurs only during lactation and is a consequence of lactostasis - stagnation of milk in the mammary gland. But no. Mastitis also occurs in non-lactation mastitis, and it is called non-lactation mastitis.
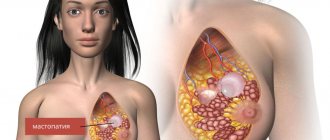
The cause of its occurrence is the same pathogenic microorganisms. Most often Staphylococcus aureus and Streptococcus. They live in the body of all living beings, but under certain conditions their numbers increase and the inflammatory process begins. The causes of mastitis in non-breastfeeding women include hormonal imbalance, breast diseases, including fibrocystic mastopathy, poorly performed plastic surgery, and acute infectious diseases. Often breast mastitis in a non-breastfeeding woman begins as a result of the penetration of an infectious pathogen into the breast tissue through a puncture of the nipple, that is, during piercing. Too rough sexual games, in which the partner touches the nipples with his teeth, can also cause mastitis in nulliparous girls, especially if they cannot boast of good immunity. A furuncle (purulent pimple) in the nipple area is another entry point for infection. And the causes of mastitis in nursing mothers are not so extensive. Usually this is advanced lactostasis, when a woman’s milk stagnates in a certain area of the mammary gland, the baby cannot absorb this lactostasis, and the woman cannot express it. After a few days, an infection penetrates there, milk is a breeding ground for pathogens, and an acute inflammatory process begins.
Although the causes of mastitis in nursing and non-breastfeeding women are different, the ways of diagnosing the disease and methods of treating it are the same. First, medicinal pathogens are killed by antibacterial agents (for example, Dicloxacillin, Cephalexin, Augmentin, Clindamycin). With advanced processes, treatment of mastitis in a non-breastfeeding woman comes down to opening the purulent cavity and cleansing it, and sometimes even removing part of the mammary gland. Naturally, this intervention may subsequently negatively affect lactation. And relapses of mastitis often occur. To get off easier and prevent complications, you need to know the signs of mastitis in non-breastfeeding women and consult a doctor in a timely manner. So, the first sign is a painful area of the mammary gland. With mastopathy, or cyclic engorgement of the mammary glands, the pain is dispersed, and if the breasts become engorged, it is entirely and not so clearly. With mastopathy, the skin of the breast does not turn red and the body temperature does not rise. These are usually the only symptoms mastitis has in non-breastfeeding women.
What to do? You need to be examined, but an experienced doctor will immediately understand what’s going on. The diagnosis can be confirmed using an ultrasound examination and analysis of nipple discharge. By the way, based on this analysis, it is possible to select suitable antibiotics for mastitis in non-lactating women. Until this moment, if a woman does not have problems with the intestines and stomach, it is possible to get rid of pain. To do this, you should use painkillers with an anti-inflammatory effect, for example, Ibuprofen, Naproxen, Ketoprofen. These are the active ingredients that are included in the drug. Commercial names of drugs may be different, for example, “Nurofen”, “Nalgesin”, “Ketonal”. But taking these drugs is not a way to treat mastitis in non-breastfeeding women, only one of the components. Even if your pain has subsided after taking the drug, this is not a reason not to go to the doctor. And long-term uncontrolled use of painkillers is fraught with serious consequences for health.
It is also better not to use folk remedies before visiting a doctor. After all, if you really have mastitis, then some of the known methods may be contraindicated for you. For example, you should not use warm compresses for mastitis.
Infected mastitis in a non-breastfeeding woman always has clear symptoms and specific signs identified by ultrasound. If the doctor noted during an ultrasound examination that an abscess has already formed in your chest - a purulent cavity, then you will need to at least take antibiotics. Exclusively antibacterial treatment is allowed for abscess sizes up to 3 cm. If more than 3 cm, surgical intervention cannot be avoided.
These are the types of problems that can arise even in a nulliparous woman. Well, the best prevention of mastitis in lactating and non-breastfeeding women is maintaining personal hygiene, avoiding nipple injuries, and timely treatment of acute infectious diseases.
Acute and chronic mastitis
Considering the severity of the pathological process and its duration, two forms of this disease can be distinguished.
In acute non-lactation mastitis, a woman is worried about minor discomfort in the mammary gland, which may be accompanied by redness of the skin in this area. As the disease progresses, there is discomfort in the axillary region, which is associated with the involvement of regional lymph nodes in the pathological process. Sometimes the temperature rises and chills appear. All these symptoms fully characterize acute mastitis in non-lactating women. Signs of mastitis indicate serious changes in a woman’s body, so you should not self-medicate. You should consult a doctor immediately.
Chronic non-lactation mastitis outside the period of exacerbation is rarely a concern. However, a dense infiltrate may form in the area of inflammation. Some patients note the appearance of chest pain of varying intensity, which radiates to the arm or shoulder. Such symptoms intensify before the start of the cycle. When the pathological process worsens, fistula tracts with purulent contents open. Externally, the disease resembles cancer in all its symptoms. Therefore, you should not hesitate or put off visiting a doctor. Lack of proper therapy can complicate mastitis in non-breastfeeding women. Treatment with antibiotics minimizes the risk of negative consequences.
Prognosis and prevention
With timely treatment of non-lactation mastitis, the prognosis is quite favorable. However, if therapy is not started on time, the woman may face complications such as:
- abscesses of internal organs;
- inflammation of the lymph nodes;
- transition to a chronic form (with acute mastitis in a non-breastfeeding woman);
- sepsis.
A healthy lifestyle is the best prevention of mastitis
Prevention of the disease includes timely treatment of various diseases, implementation of measures aimed at strengthening the immune system, normalizing hormonal levels and preventing injuries to the mammary gland.
In addition, you need to go for preventive examinations to a mammologist. He will be able to detect the pathological process at the earliest stages, because he knows the symptoms and treatment of non-lactation mastitis in non-lactational mastitis better than other specialists.
Other forms of the disease
Non-lactation mastitis very rarely develops into more complex purulent stages and responds well to therapy. If this is a physiological condition, treatment is not required at all. The symptoms of this disease are largely determined by its form.
- Serous mastitis in non-lactating women is usually a borderline condition. Symptoms are often absent and more reminiscent of mastopathy. Some women note moderate swelling and swelling of the breasts, and a slight increase in temperature.
- Infiltrative non-lactation mastitis has a more pronounced clinical picture. Patients complain of increased temperature and heaviness in the mammary gland. The breasts may be hot to the touch.
- Purulent mastitis in non-lactating women is characterized by pronounced symptoms: chest pain, swelling, high fever. The patient's condition deteriorates sharply. This is due to the entry of toxins into the blood from a purulent focus of inflammation. The disease in this form resembles a pathological condition that develops during lactation.
Depending on the form of the disease, the doctor prescribes appropriate treatment. However, to determine it, it is necessary to undergo a medical examination.
Symptoms and diagnosis
Mastitis not associated with lactation rarely develops. Its symptoms are the same as those of the lactational one, but only less pronounced.
The disease is characterized by:
- headache;
- body aches, chills;
- general weakness;
- swollen lymph nodes;
- soreness of the glands;
- sensation of compaction upon palpation.
The diagnosis is determined based on the following tests:
- clinical blood test;
- general urine analysis;
- determination of blood glucose levels.
Ultrasound is the main instrumental diagnostic method. It is used in differential diagnosis and in long-term treatment of acute forms. A feature of the disease is the frequent degeneration of mastitis into an oncological tumor. Therefore, women will be examined not only by a surgeon, but also by a mammologist. The tissues of the opened abscess are subjected to histological examination.
Diagnostic measures
Confirming the disease is usually not difficult. The diagnosis of “non-lactation mastitis” in non-lactating women is determined on the basis of complaints and clinical picture. The doctor may also order an ultrasound and biopsy of the affected area. In particularly serious cases, microbiological examination of secretions from ulcers is required. In addition, a complete examination of the patient is carried out to determine the underlying disease that caused the hormonal imbalance.
Symptoms of mastitis in non-breastfeeding women
If a woman has already stopped breastfeeding, she is at risk of developing mastitis. This is not something out of the ordinary, it is a very common disease affecting a different segment of women. If a woman has never given birth, she is also at risk, but to a lesser extent, since the extent of the damage has not yet developed. That is, a woman can succumb to a cold, illness, flu, but if she has not previously suffered even from the symptoms that cause the disease, she has nothing to fear.
Basic principles of therapy
Treatment of the disease depends on its form, stage and the presence of concomitant ailments. As mentioned above, mastitis in non-lactating women is sometimes a physiological norm. In this case, specific therapy is not required; they are limited to dynamic monitoring of the state of health. Severe disease is treated with antibiotics and antihistamines. All drugs are selected individually.
Depending on what caused mastitis in non-breastfeeding women, treatment may be prescribed simultaneously by several specialists. If the disease occurs due to hormonal imbalances, therapy is selected by an endocrinologist. When mastitis is a consequence of an infection in the chest or injury, consultation with a surgeon is required.
Treatment methods
The choice of treatment for non-lactation mastitis depends on the causes of the disease, as well as the severity of the pathological process. In any case, treatment for mastitis in nulliparous women should begin as early as possible. In this case, you cannot use wait-and-see tactics, as with the lactation form of the disease. Otherwise, the woman may face dire consequences.
Traditional methods are often used in the treatment of mild forms of mastitis
If the pathology occurs in a mild form, then the doctor may recommend the patient to use remedies made according to traditional medicine recipes, as well as homeopathic medicines.
The woman is required to be prescribed antibacterial medications. The choice of the most suitable one is made by the doctor based on the results of bacterial culture. After taking antibiotics, already on the 2-3rd day, signs of mastitis in a non-breastfeeding woman may partially or completely disappear. However, this does not mean that the course of treatment needs to be interrupted. The medication must be taken for 7-10 days, otherwise the woman will experience a relapse.
Important! Unfortunately, antibiotics negatively affect not only pathogenic bacteria, but also healthy human microflora. That is why, in order to avoid the development of dysbiosis, the patient must use probiotics throughout the entire course of treatment and for some time after it.
For mastitis, antibiotic therapy is mandatory
To eliminate pain from mastitis in a non-breastfeeding woman, analgesics can be used. To eliminate the inflammatory process, a specialist may prescribe drugs from the NSAID group.
Advice! To speed up the removal of toxins from the body and eliminate the unpleasant symptoms of non-lactation mastitis, the patient should drink at least 2 liters of water per day.
Severe cases of the disease may require surgical intervention. In this case, the surgeon opens the lesion, cleans it of pus and drains it.
Surgery for non-lactation mastitis is performed under general anesthesia or using local anesthesia (depending on the extent of the intended surgical intervention). At the end of the procedure, a suture is placed on the chest. In this case, special cosmetic threads are used, so a woman does not have to worry about scars forming on her breasts.
In the most advanced cases, surgery may be required to eliminate mastitis.
Important! In smoking patients, body tissues are much less saturated with oxygen than in those who lead a healthy lifestyle. This may negatively affect the wound healing process. Therefore, during treatment and during the rehabilitation period, it is better for a woman to give up the addiction.
After the basic treatment measures have been taken, the patient is prescribed hormonal drugs. Their choice is made based on the age, height, weight and phenotype of the woman. You need to take these medications for several months.
To prevent relapse, a specialist may prescribe immunostimulating medications, as well as vitamin and mineral complexes.
Treatment with folk remedies
Along with conservative therapy, doctors recommend using traditional medicine. At the initial stages of the disease, you can include procedures for washing the affected breast with a special infusion. To prepare it, you need two tablespoons of a dry mixture of chamomile and yarrow flowers (1:4) poured into 0.5 liters of boiling water. This infusion has a disinfectant and anti-inflammatory effect.
To relieve swelling, you can prepare a honey cake. To do this, you need to mix a tablespoon of honey with two tablespoons of flour and knead the dough. The cake must be applied to the affected area and covered with gauze on top. Such a compress must be kept for at least 10 hours.
Mastitis in non-lactating women, the symptoms of which are described in this article, requires qualified treatment. Warming compresses should not be used. High temperatures can cause suppuration. The use of traditional recipes is permissible only after consulting a doctor.
Treatment of mastitis
After the examination, the reason why non-lactation mastitis appeared is determined.
If it is caused by an infectious disease, the treatment will contain a certain range of mild antibiotics. It is impossible to do without them. If the cause of mastitis is a weakened immune system, treatment involves taking herbal medicines and vitamins. Mastitis caused by injury or pressure can be treated with compresses and properly selected underwear. Treatment is prescribed by an endocrinologist if the problem lies in dysfunction of the thyroid gland or ovaries. In this case, hormonal drugs may be prescribed. The course of taking hormonal drugs lasts at least six months. Mastitis in a non-breastfeeding girl should not be treated with chemotherapy or biopsy. No fluid is required for breast examination.
Diagnostics
Diagnosis of non-lactation mastitis can be carried out exclusively within the walls of a medical institution. Before visiting a doctor, the patient should stop taking any medications (except vital ones).
Diagnosis of pathology always begins with an examination of the patient, questioning and careful collection of her medical history. Before treating non-lactation mastitis, your doctor may prescribe:
To confirm the diagnosis of non-lactation mastitis, a woman must undergo a series of studies. During the diagnosis, the doctor must not only confirm the fact of the presence of the disease, but also identify the reasons why it arose. Thanks to this, you can choose the most effective treatment method and prevent relapse.