Fungal infection of the genital organs (candidiasis) is an infectious and inflammatory process of the mucous membrane, spreading to the vulva and cervix. These are gynecological diseases, the causative agent of which is Candida fungi, which are found in the body of any person.
A fungal infection may not manifest itself for a long time, however, under certain “favorable” circumstances, it quickly activates its activity. Yeast fungus in women: symptoms and causes
Many women are at risk of contracting vaginal fungus, so it is important to know the cause of the disease in order to identify it in the early stages and begin proper treatment.
According to medical statistics, an infection caused by yeast fungus occurs in almost every fourth woman.
A fungal infection occurs as a result of weakened immunity, during which the fungus rapidly multiplies and affects the mucous membrane of the female genital organs and gastrointestinal tract.
Causes of yeast in a smear
The immediate reason for detecting yeast in a smear is the yeast itself that is present there.
These are fungi of the genus Candida.
They are transmitted sexually.
In addition, the development of endogenous infection is possible.
The fact is that candida is part of the normal microflora.
These fungi have low immunogenicity.
Therefore, they exist on the skin, mucous membranes, in the genital and digestive organs.
However, there are no symptoms.
Problems only begin to arise when there is excessive growth of fungal flora.
Why does yeast appear in the smear?
There are two reasons for detecting yeast cells:
- infection with candidiasis from a sexual partner;
- creating conditions in the body that are favorable for the growth of fungi.
Favorable conditions mean:
- decreased immunity;
- destruction of microflora competitive for candida with antibiotics (candidiasis often manifests against the background of antibiotic therapy for bacterial infections);
- insufficient hygiene of the reproductive organs, accumulation of gland secretion products and exfoliated cells on them;
- Fever – creates warm and humid conditions that are optimal for yeast growth.
In most cases, the disease is not dangerous.
It is fraught with only unpleasant sensations.
But complications do not usually develop in immunocompetent patients.
At risk are elderly, seriously ill and debilitated patients.
As well as persons with diabetes, immunodeficiency conditions or HIV.
Under what symptoms can yeast be detected in a smear?
Typically, women do not go to the doctor or laboratory just like that.
They are forced to seek medical help by the symptoms that arise.
Here is a list of clinical signs in which the probability of detecting yeast in a smear is quite high:
- redness of the genitals;
- severe itching;
- accumulation of white plaque;
- curdled vaginal discharge;
- swelling;
- sour smell;
- the appearance of erosions and cracks.
Elements of the rash are usually limited to red spots and papules.
In severe cases of candidiasis, erosions, ulcers and pustules occur.
The spots become larger.
In addition to the vagina and vulva, the surrounding skin may also become inflamed.
Candidiasis usually does not spread upward.
What tests detect yeast?
A smear is just a way to take clinical material.
To find yeast in it, various laboratory tests are used.
Most often this is a microscopic examination.
Less commonly, fungal culture or PCR.
Microscopy
Discharge is taken from the genitals or plaque accumulated on the surface is collected.
A preparation is prepared from it, which is examined under microscope magnification.
Staining is usually done with potassium hydroxide.
It allows you to “clarify” the drug, making it more convenient for study.
In the field of view of the microscope, the doctor discovers:
- increased number of leukocytes - inflammatory cells;
- budding fungal cells;
- fungal elements (spores, pseudomycelium).
In combination with characteristic clinical signs, this is a sufficient basis for making a diagnosis.
This does not determine:
- type of fungus (there are many candida);
- number of fungi.
Regarding the quantity, only one thing can be said: if yeast begins to appear in the field of view, this indicates that its concentration is not less than 10 in 3 per ml.
As you can see, the test is not the most informative.
However, for most patients this is sufficient.
In the vast majority of cases:
- the type of fungus is candida albicans;
- the amount of yeast has no clinical significance and does not affect the choice of treatment regimen.
Therefore, compelling reasons are needed to prescribe additional tests.
They are usually required if:
- candidiasis is not treatable;
- the disease becomes chronic or recurrent.
Then it is necessary to determine the type of fungus, its quantity, as well as predisposing factors (concomitant diseases that provoke candidiasis).
Sowing
The biomaterial obtained as a result of the smear is sown on a nutrient medium.
After a few days, fungi grow.
The emerging colonies have a characteristic appearance.
In addition, different fungi differ in enzymatic, immunological and other properties.
Cultures provide the doctor with valuable information:
- determines the type of fungus;
- estimates the amount in colony-forming units;
- shows the sensitivity of yeast to antimycotics, allowing you to choose the best one for the treatment of candidiasis (the risk of treatment failure is reduced to a minimum).
PCR
The molecular biological method has both advantages and disadvantages.
Such diagnostics are cheaper and take less time.
It allows you to accurately determine the type of fungus and also gives quantitative indicators.
The examination is usually carried out simultaneously on 5-8 of the most common yeast species.
During PCR, a DNA fragment specific to a particular candida is detected.
On the other hand, sowing is still more preferable.
The fact is that both studies are not routine.
They are prescribed strictly according to indications.
Namely, they are carried out when relapses occur or difficulties in treating a yeast infection occur.
But, unlike PCR, culture makes it possible to assess sensitivity to antimycotics.
Therefore, after this study, the likelihood of a cure is higher.
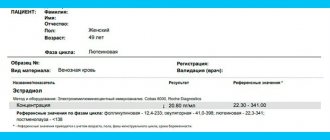
Blood analysis
Candidiasis is diagnosed by a blood test.
This test is not used for the primary diagnosis of infection.
It is used solely to assess the risk of complications.
Candida has low immunogenicity.
With superficial (uncomplicated) candidiasis, immunoglobulins in the blood are not detected.
They begin to appear only with deep (invasive) candidiasis.
It differs in that internal organs are involved in the pathological process.
This form of yeast infection develops only in patients with immunocompromised conditions.
The presence of IgG in the blood does not confirm invasive candidiasis.
But if IgG is not detected, this practically guarantees its absence.
Thus, this test has a high negative predictive value.
At the same time, its results only refute invasive candidiasis, but do not confirm it.
If antibodies are detected, additional tests are needed to assess the extent of the yeast infection.
What is candida mycelium and spores?
Only medical laboratory workers can see the mycelium threads in a smear, since the microscopic size of this substance is not accessible to the naked human eye.
Detection of mycelium is an alarming signal indicating the proliferation of pathogenic microflora in the vagina.
Therefore, it is important for a woman to know what mycelium threads are in test results and how to effectively solve the problem.
What is fungal mycelium?
The mycelium in the smear is thin, branching threads that are the plant part of the Candida fungus and feed it. This is a sign of the development of candidiasis (thrush) in the body.
If mycelium threads are found in the smear , it means that the fungus is in an active stage of reproduction: the fungus grows, feeds and destroys beneficial microflora.
Even a single fungal mycelium in a smear is an indicator of candidiasis.
What does the presence of disputes mean?
Spores of the yeast-like fungus Candida are found in the smear of a carrier of the disease. These cells are embryos separated from the mother's body. When favorable conditions arise, the spores begin to grow and produce offspring. A sluggish process develops into a disease. If fungal spores are found, it means that candidiasis will begin in the near future.
Causes of spores
Yeast microorganisms live peacefully in small quantities in the vagina and are part of its normal microflora. Active reproduction of fungi begins under favorable conditions, which are provoked by the following factors:
- periods of hormonal surges with fluctuations in estrogen levels: puberty, menopause, pregnancy;
- taking antibiotics, corticosteroids, hormonal contraceptives;
- tuberculosis, STDs, diabetes;
- external factors: tight underwear, poor intimate hygiene , heat, use of low-quality pads, contact with a patient, microflora disturbance, improper hygiene;
- decreased immunity due to stress, postoperative condition.
Why are disputes dangerous?
The danger of the presence of fungal spores in a smear is the likelihood of the pathology transitioning to the chronic stage. Failures in the body cause exacerbation and manifestation of the disease. Fungal spores can trigger the development of more serious problems:
- to intrauterine infection of the fetus;
- to infection of the child when passing through the birth canal;
- to the development of oncology;
- to cervical erosion;
- to the addition of infections caused by microflora disturbances.
Possible symptoms
The growth of yeast microflora in the vagina is accompanied by the following symptoms:
- burning and itching in the genitals;
- pain during sex;
- painful urination;
- whitish, cheesy discharge with an unpleasant odor.
The intensity of such manifestations depends on the stage of fungal reproduction, as well as on the individual characteristics of the organism. Some women, even at the initial stage of thrush, experience unbearable itching. For other women, a sign of the disease is mild discomfort.
Treatment method
Therapy for candidiasis includes suppression of pathological microflora, restoration of the body's immunity, and normalization of the gastrointestinal tract.
Drug therapy
Taking antifungal drugs aimed at destroying spores and threads of Candida mycelium forms the basis of all therapy. The treatment complex consists of taking systemic (tablets) and local (suppositories, ointments) drugs.
Systemic treatment is used at the chronic stage of the disease; local drugs are effective only at the beginning of fungal proliferation.
The following systemic and local agents are most effective:
- Tablets, capsules: “Diflucan”, “Diflazon”, “Flucostat”, “Ketonazole”, “Nystatin”.
- Suppositories, ointments: “Terzhinan”, “Clone-D”, “Pimafucin”, “Natamycin”.
Detection of yeast fungi in smears suggests simultaneous treatment of sexual partners. Failure to treat a man in 100% of cases leads to re-infection of his partner with candidiasis.
Treatment is carried out strictly as prescribed by the doctor. Self-selection of drugs develops the fungus resistance to the substance and complicates further treatment.
After the destruction of yeast fungi, it is necessary to restore the microflora and populate the vagina with beneficial bacteria. Taking lacto- and bifidobacteria is a prerequisite for successful treatment of thrush.
Beneficial bacteria begin to multiply in the vagina, forming a “living shield” against pathogenic microflora. The following probiotics, symbiotics, and bifid drugs are widely used:
- “Acilact” in the form of a suppository. It is used intravaginally 2 times a day.
- “Acipol” (symbiotic capsules). Taken 3 times a day.
- Trilact consists of three types of bacteria and is most effective for thrush.
- “Kipacid” is a symbiotic complex with immunoglobulin.
Physiotherapy
Physiotherapeutic procedures in the treatment of fungus have a bacteriostatic, anti-inflammatory, and antipruritic effect. Systemic treatment includes:
- inductothermy;
- darsonvalization;
- magnetic therapy;
- mud treatment;
- UV irradiation;
- microwave therapy;
- electrophoresis with zinc;
- laser therapy;
- ozone therapy.
Folk remedies
There are traditional methods for treating candidiasis:
- Douching, baths with decoctions of chamomile, yarrow, sage, calendula.
- Tampons with kefir, honey solution, garlic juice.
Taking a smear on the flora and deciphering it
A smear from the vagina, urethra and cervix is taken to assess the microflora. A healthy environment is 95-98% populated by lactobacilli (Dederlein bacilli). The remaining percentage is opportunistic flora that lives peacefully in the genitals.
When conditions are favorable, pathogens begin to multiply, replacing beneficial bacteria and causing inflammation. A smear allows you to assess the quantity and quality of bacteria living in the vagina, as well as the level of acidity of the environment.
Deciphering a smear is determining the specific amount of bacteria it contains. Ideally, the main content should be Dederlein bacilli, the rest should be in minute quantities, and some microorganisms should not be present at all.
The total number of bacteria is indicated in numbers or by “+” signs in the range from 1 to 4. A minus sign indicates the absence of cells. The analysis form may contain the entry “not found” or “abs” (absence in Latin).
The results of the smear and the norms for the content of rods in them:
| Microflora content | Designation in the analysis form | Norm |
Increased yeast in the smear
If yeast is detected, it does not mean you are sick.
You need to pay attention to the following things:
- are there any symptoms of candidiasis;
- how the research was conducted.
Candida is a normal inhabitant of the human reproductive organs.
If there is a small amount of fungi on the skin and mucous membranes, it is not scary.
There is no point in treatment for:
- no symptoms of candidiasis;
- detection of this infection in an amount less than 10 to 3 degrees CFU or DNA copies per ml (depending on whether the diagnosis was carried out by culture or PCR).
At the same time, detection of yeast by microscopy is a clear indication for therapy.
Because mushrooms come into view only when their number is increased.
Yeast in a smear of men
Male patients are much less likely to suffer from candidiasis.
However, such cases also happen to them.
There are two reasons:
- infection from a woman suffering from vulvovaginal candidiasis;
- creating favorable conditions for yeast growth (usually weakening the immune system or antibiotic therapy).
In men, the most common clinical form of the disease is candidiasis balanoposthitis.
Urethritis is diagnosed much less frequently.
If present, it usually complicates inflammation of the head of the penis.
Symptoms are generally the same as in women:
- itching;
- redness;
- white thick deposits;
- papules, erosions, fissures, pustules, depending on the severity of the infection.
Similar tests are prescribed.
Yeast can be detected by microscopy.
To clarify the type of fungi, PCR or cultural testing is used.
Prevention of genital yeast fungus
In order not to encounter problems of infection with thrush, you should consider and follow
some rules of personal hygiene. To begin with, you should definitely take a shower or bath every day, then dry yourself thoroughly and try to change the towel at least once every two days. For such a task, a woman should have a separate intimate towel.
Underwear should not be too tight-fitting, made of natural fiber, with a breathable structure.
If you are suffering from an infectious disease and undergoing a course of antibiotics, you should definitely take a course of probiotics, which will keep your gastrointestinal tract in good condition without causing the proliferation of Candida fungus and other bacteria of internal and intimate organs.
What to do if fungi are found in a smear?
Need treatment.
In most cases, therapy is quick and successful.
Often one tablet is enough to get rid of the disease.
If the disease is severe or constantly worsens, therapy takes longer and is carried out with several drugs.
In any case, it is not you, but your doctor, who will decide what to do next.
He is guided by the results of tests, including additional ones (for sexually transmitted infections and diseases that are predisposing factors).
Education:
- University of Illinois, Chicago (UIC), 1972-1976
- Chicago College of Osteopathic Medicine, Midwestern University, 1978-1982
- Chicago Osteopathic Hospital, 1982-1985, residency in family medicine. Senior Resident, 1984-1985
- Certified American College of Osteopathic General Practitioner Training, July 1985
- Licensed Physician and Surgeon in the State of Illinois
You can read more details here
PS And remember, just by changing your consciousness, we are changing the world together! © econet
Treatment of yeast in a smear
The easiest way to cure candidiasis is to take a fluconazole tablet.
It is taken once.
Dose – 150 mg.
Usually, after this, the symptoms of inflammation quickly disappear.
This scheme is used when:
- no complications;
- mild clinical course of candidiasis (and this is the majority of cases);
- form of the disease caused by Candida albicans rather than atypical Candida.
Itraconazole can be used as an alternative drug.
But they have to undergo treatment longer.
You can also treat yeast in a smear with local medications.
But most patients find them less comfortable.
Causes:
- the need for daily use;
- the course of treatment lasts 1 week, not 1 day;
- candles and creams stain linen: both underwear and bed linen;
- therapy may be more expensive.
On the other hand, local exposure has an obvious advantage.
Many antifungal medications are harmful to the liver.
When used locally, any health risks are eliminated and systemic side effects do not develop.
Folk remedies for thrush in women
Traditional treatments help in the fight against infection:
- Mix chamomile, burdock, elecampane, and St. John's wort herbs in equal parts, brew for an hour, pass through a filter, then take 120 ml every day in the morning, afternoon and evening. Elecampane and burdock can be brewed and used for douching the vagina before bed. Before this, you need to wash everything inside well, then douche and in the morning wash everything inside the vagina again.
- Fir oil and cocoa butter should be mixed 1:10. Then this entire mixture needs to be boiled for about 10 minutes and left to cool to a temperature of 35-36 C. Then you need to make tampons from cotton wool or a bandage for insertion into the vagina, moisten them in the resulting mixture and leave overnight. It is advisable to wear a panty liner so as not to stain your underwear if the mixture leaks.
- Dilute copper sulfate with water according to - 4 tsp. per liter of hot water. The slightly infused solution should be further diluted with water, 2 tbsp. for 2 liters of water. A diluted solution can also be used for douching, rinsing the labia, or washing after taking a shower.
Yeast in a smear during pregnancy
During pregnancy, yeast is detected quite often.
This is due to the fact that due to hormonal changes, immunity decreases.
As we have already said, candida in this case begins to multiply quite quickly.
She's just waiting for her immune system to fail.
But treatment of yeast during this period cannot be carried out with systemic medications.
Because they can harm the fetus.
Preference is always given to local treatment.
Use creams, ointments or suppositories containing:
- clotrimazole;
- miconazole;
- Butoconazole
Of course, these drugs are not used simultaneously.
Only one of them is selected.
You need to put candles on at night, once a day.
The standard course of treatment lasts 7 days.
Biography:
I was born and raised in the inner city of Chicago, Illinois. I had an ordinary childhood. Already during my school years, I became interested in issues of health care and disease prevention. When I was in my twenties, I worked as a pharmacist in a doctor's office. While working at the Illinois Eye Bank, I was responsible for accepting donor eyes that would be used for corneal transplants. I also worked at the Kidney Bank.
I began seeing patients on my own at my private disease prevention clinic in Schaumburg, Illinois, in 1985. I was the only practicing doctor. My work included routine screenings, physical examinations of schoolchildren, and appointments with patients with chronic illnesses. I prescribed medications, but eventually realized they were not effective.
In the early 1990s, I began exploring the field of natural medicine. After seeing dramatic improvements from changing patients' diets and increasing physical activity, I made adjustments to my medical practice.
Why is there no effect from treating yeast in a smear?
Insufficient effect of treatment means the following:
- symptoms do not disappear;
- there is no less yeast in the smear;
- the symptoms go away, but after a while a relapse occurs.
Such unfavorable situations may be due to the following reasons:
- the disease is caused by atypical candida (not albicans) - they are less susceptible to traditionally used drugs;
- the treatment was carried out incorrectly (perhaps you got a bad doctor);
- the person tried to treat himself;
- candida turned out to be resistant to the drug used;
- there are profound immunity disorders or other predisposing factors (diabetes, poor hygiene, local use of glucocorticoids, etc.).
If there is no effect of treatment or relapse, culture for candida or PCR is performed.
The patient is examined for HIV, diabetes, the state of immunity is assessed, and checked for concomitant sexually transmitted infections.
The treatment regimen usually changes.
Antimycotics of another pharmacological group are prescribed.
Using PCR, doctors monitor the dynamics.
They determine whether the concentration of yeast in the smear is decreasing.
In addition to the main treatment, enzymes, immunomodulators, local antiseptics and antifungal drugs are prescribed.
After a course of therapy, clinical and laboratory monitoring is required.