Pregnancy and childbirth are a difficult process for a woman. A global restructuring is taking place in the body, life support systems are working at double capacity. But even if there were no problems during pregnancy, they may arise during delivery. Doctors often use the drug Oxytocin.
Sometimes it happens that labor does not occur at the scheduled time and there is a threat to the life of the child and the mother. Doctors use the drug “Oxytocin” for stimulation. How does it work, and what contraindications does it have?
The concept of a hormone
Oxytocin is an endogenous hormone that is synthesized in every female body.
Responsible for the state and functioning of the endocrine system, metabolism and secretion of the genital organs. The hypothalamus is responsible for creating the hormone itself. The formed substance enters another part of the brain - the pituitary gland, where it accumulates, and then, when a certain concentration level is reached, oxytocin is released into the blood. The hormone is responsible for all processes occurring in the female body: the menstrual cycle, the course of pregnancy. Its performance also depends on this. Peak values are formed at the end of the third semester, which starts the processes of preparation for labor. The hormone reaches especially high levels at night, which is why labor most often begins at night.
Special cases
In some cases, postpartum uterine contractions have features that it is better for a woman to know about in advance so as not to be scared and be prepared for the unexpected.
After the second birth
Most often, uterine contractions after the second birth occur much more intensely. Therefore, in the first days, the chest may be very sore and swollen, especially during feeding, and also breaks the lower abdomen and perineum. The sensation may be so painful that your doctor will prescribe a pain reliever. It is not recommended to select medications and folk remedies on your own, as they can negatively affect lactation.
After artificial birth
Contractions of the uterus after artificial birth also cause some concern, since the body does not perceive them properly. Therefore, in most cases, medications are prescribed or folk remedies are used to speed up the process.
Another danger is severe bleeding, which is not normal: it needs to be stopped as quickly as possible. After an artificial birth, the recovery period depends on the period at which the pregnancy was terminated. Typically, the time of uterine contraction ranges from 3 days to 2 weeks, no more if everything goes without complications.
The female body, despite the modern development of science and medicine, still remains a mystery. The uterus is one of its most amazing organs. Only she has such amazing elasticity and can change sizes on such a scale. To help her recover faster, you need to perform various physical exercises and consult a doctor in a timely manner. Folk remedies that help increase uterine contractions during this period should be used with extreme caution. There are standards with which you need to constantly compare your feelings, the composition of the discharge and the timing.
Author's article
For several weeks after childbirth, while the uterine mucosa (endometrium) is being restored, the young mother continues to have discharge from the genital tract. What are these discharges and in what cases can they become a sign of trouble?
Discharge from a woman's genital tract after childbirth is called lochia. Their number decreases over time, which is explained by the gradual healing of the wound surface that forms on the endometrium after the separation of the placenta.
Lochia consists of blood cells (leukocytes, erythrocytes, platelets), plasma sweating from the wound surface of the uterus, dying epithelium lining the uterus, and mucus from the cervical canal. Over time, the composition of the lochia changes, and therefore their color also changes. The nature of lochia should correspond to the days of the postpartum period. In the first days after childbirth (4-5 days after vaginal delivery and 7-8 days after cesarean section), the woman is in the maternity hospital in the postpartum department under the supervision of medical personnel. But after a woman is discharged home, she controls her condition herself, and her task is to consult a doctor if necessary. The amount and nature of discharge can speak volumes, and it is important to notice alarming symptoms in time.
In the birth block
For the first 2 hours after birth, the woman is in the maternity ward - in the same box where the birth took place, or on a gurney in the corridor.
It is good if the discharge immediately after childbirth is bloody, quite abundant, amounts to 0.5% of body weight, but not more than 400 ml, and does not lead to a violation of the general condition.
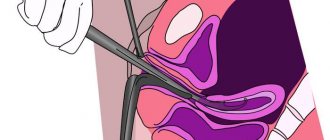
To prevent postpartum hemorrhage, immediately after childbirth, empty the bladder (discharge urine through a catheter) and put ice on the lower abdomen. At the same time, drugs that contract the muscles of the uterus (Oxytocin or Methylegrometril) are administered intravenously. By contracting, the uterus closes open blood vessels at the placenta attachment site, preventing blood loss.
Note! In the first two hours after birth, a woman is in the maternity ward under the supervision of medical personnel, because this period is dangerous due to the occurrence of so-called hypotonic uterine bleeding, which is caused by a violation of the contractile function of the uterus and relaxation of its muscles. If you feel that the bleeding is too heavy (the diaper is wet, the sheet is wet), you should immediately tell someone from the medical staff about it. It is important to know that the woman does not experience any pain, but bleeding quickly leads to weakness and dizziness.
Also, in the first 2 hours, bleeding may occur from tears in the tissue of the birth canal if they have not been sutured, so it is important that the doctor carefully examine the vagina and cervix after childbirth. If any rupture was not completely sutured, a hematoma (a limited accumulation of liquid blood in the tissues) of the perineum or vagina may occur. In this case, a woman may experience a feeling of fullness in the perineum. In this case, it is necessary to open the hematoma and re-suturing the rupture. This operation is performed under intravenous anesthesia.
If the first 2 hours after birth (early postpartum period) went well, the woman is transferred to the postpartum ward.
In the postpartum ward
It’s good if in the first 2-3 days the lochia is bloody, it is quite abundant (about 300 ml in the first 3 days): the pad or diaper is completely filled within 1-2 hours, the lochia may be clotted and have a musty smell like menstrual flow. Then the number of lochia decreases, they acquire a dark red color with a brown tint. Increased discharge when moving is normal. In the postpartum department, the doctor makes a daily round, during which, among other indicators of the woman’s condition, he evaluates the nature and amount of discharge - for this he looks at the discharge on the pad or pad. A number of maternity hospitals insist on using diapers, because this makes it easier for the doctor to assess the nature of the discharge. Usually the doctor checks with the woman the amount of discharge during the day. In addition, in the first 2-3 days, discharge may appear when the doctor palpates the abdomen.
To prevent postpartum hemorrhage, it is important to follow the following recommendations:
Empty your bladder in a timely manner. During the first day, you need to go to the toilet at least every 3 hours, even if you don’t feel the urge to urinate. A full bladder prevents normal uterine contractions. Breastfeed your baby on demand. During feeding, the uterus contracts as irritation of the nipples causes the release of oxytocin, a hormone produced in the pituitary gland, an endocrine gland located in the brain. Oxytocin has a contractile effect on the uterus. In this case, the woman may feel cramping pain in the lower abdomen (in multiparous women they are stronger). Discharge increases during feeding. Lie on your stomach. This not only prevents bleeding, but also prevents the retention of discharge in the uterine cavity. After pregnancy and childbirth, the tone of the abdominal wall is weakened, so the uterus can deviate posteriorly, which disrupts the outflow of secretions, and in the position on the stomach, the uterus approaches the anterior abdominal wall, the angle between the body of the uterus and the cervix is eliminated, the outflow of secretions improves. 3-4 times per day. day, place an ice pack on the lower abdomen - this measure helps to improve the contraction of the muscles of the uterus and uterine vessels.
Women whose uterus was overstretched during pregnancy (in pregnant women with a large fetus, in multiple pregnancies, in multiparous women), as well as those in whom labor occurred with complications (weakness of labor, manual separation of the placenta, early hypotonic bleeding) in the postpartum period, the drug Oxytocin is prescribed intramuscularly for 2-3 days so that the uterus contracts well.
If the amount of discharge increases sharply, you should definitely consult a doctor.
Note! If the amount of discharge has sharply increased, you should definitely consult a doctor, as there is a danger of late postpartum hemorrhage (late postpartum hemorrhage includes those bleeding that occurred 2 or more hours after the end of labor). Their reasons may be different.
Bleeding may be a consequence of retained parts of the placenta if it was not diagnosed in time (in the first 2 hours after birth). This bleeding may occur in the first days or even weeks after birth. The share of the placenta in the uterus can be detected by vaginal examination (if it is located close to the internal os and the cervical canal is patent) or by ultrasound. In this case, a portion of the placenta is removed from the uterus under intravenous anesthesia. In parallel, infusion therapy (intravenous drip administration of liquids) is carried out, the volume of which depends on the degree of blood loss, and antibacterial therapy to prevent infectious complications.
In 0.2-0.3% of cases, bleeding is caused by disorders in the blood coagulation system. The causes of these disorders can be various blood diseases. Such bleeding is the most difficult to correct, so preventive therapy started before birth is very important. Usually a woman is aware of the presence of these disorders before pregnancy.
Most often, hypotonic bleeding occurs due to insufficient contraction of the uterine muscles. In this case, the bleeding is quite profuse and painless. To eliminate hypotonic bleeding, reducing drugs are administered, blood loss is compensated by intravenous fluid administration, and in case of severe bleeding, blood products (plasma, red blood cells). If necessary, surgical intervention is possible.
If the discharge stops, you should also consult a doctor. A complication of the postpartum period, characterized by the accumulation of lochia in the uterine cavity, is called lochiometra. This complication occurs due to overstretching of the uterus and its bending backwards. If the lochiometra is not eliminated in time, endometritis (inflammation of the uterine mucosa) may occur, because postpartum discharge is a breeding ground for pathogens. Treatment consists of prescribing drugs that contract the uterus (Oxytocin). In this case, it is necessary to eliminate cervical spasm, for which No-shpa is administered 20 minutes before Oxytocin.
At home
It’s good if postpartum discharge lasts 6-8 weeks (that’s how long it takes for the uterus to develop back after pregnancy and childbirth). Their total quantity during this time is 500-1500 ml.
In the first week after childbirth, the discharge is comparable to normal menstruation, only it is more abundant and may contain clots. Every day the amount of discharge decreases. Gradually they acquire a yellowish-white color due to a large amount of mucus, and may be mixed with blood. Approximately by the 4th week, scanty, “spotting” discharge is observed, and by the end of the 6-8th week it is already the same as before pregnancy.
In women who are breastfeeding, postpartum discharge stops faster, as the entire process of reverse development of the uterus occurs faster. At first there may be cramping pain in the lower abdomen when feeding, but within a few days it goes away.
In women who have undergone a cesarean section, everything happens more slowly, since, due to the presence of a suture on the uterus, it contracts less well.
Hygiene rules during the postpartum period. Following simple hygiene rules will help avoid infectious complications. From the very first days of the postpartum period, a variety of microbial flora is found in the lochia, which, when multiplying, can cause an inflammatory process. Therefore, it is important that lochia does not linger in the uterine cavity and vagina.
During the entire period while the discharge continues, you need to use pads or diapers. Gaskets must be changed at least every 3 hours. It is better to use pads with a soft surface than with a mesh surface, because the nature of the discharge is better visible on them. Pads with fragrances are not recommended - their use increases the risk of allergic reactions. While you are lying down, it is better to use padding diapers so as not to interfere with the release of lochia. You can put a diaper on it so that the discharge comes out freely, but does not stain the laundry. Tampons cannot be used, as they prevent the removal of vaginal discharge, instead absorbing it, which can cause the proliferation of microorganisms and provoke the development of an inflammatory process.
You need to wash yourself several times a day (after each visit to the toilet), you need to take a shower every day. The genitals need to be washed from the outside, but not from the inside, from front to back. You cannot douche, because this way you can get an infection. For the same reasons, it is not recommended to take a bath.
During intense physical activity, the volume of discharge may increase, so do not lift anything heavy.
You should seek medical help in the following cases: The discharge has acquired an unpleasant, pungent odor and is purulent in nature. All this indicates the development of an infectious process in the uterus - endometritis. Most often, endometritis is also accompanied by pain in the lower abdomen and fever. Heavy bleeding appears after its amount has already begun to decrease, or the bleeding does not stop for a long time. This may be a symptom that there are parts of the placenta that have not been removed in the uterus, which interfere with its normal contraction. The appearance of cheesy discharge indicates the development of yeast colpitis (thrush). In this case, itching in the vagina may also appear, and redness sometimes occurs on the external genitalia. The risk of this complication increases when taking antibiotics. Postpartum discharge suddenly stopped . Complications are more common after a cesarean section than after a natural birth. If there is severe bleeding (several pads within an hour), you should call an ambulance rather than go to the doctor yourself.
The above complications do not go away on their own. Adequate therapy is necessary, which should be started as early as possible. In some cases, hospital treatment is required.
If complications arise after childbirth, a woman can go not only to the antenatal clinic, but also (in any case, at any time of the day) to the maternity hospital where the birth took place. This rule is valid for 40 days after birth.
The role of hormones during childbirth
The main task of oxytocin is to ensure uterine contractions. Preparation for this process occurs during pregnancy. Contraction begins thanks to receptors in the organ that are sensitive to the effects of the hormone. During pregnancy, their number increases many times and at the same time sensitivity to the hormone increases. Oxytocin affects other organs much less, since the main localization of receptors is in the uterine cavity, in other parts their number is insignificant.
Simultaneously with the increased synthesis of the hormone in the female body, the concentration of a special enzyme responsible for the utilization of the substance increases. A significant portion of oxytocin passes into the placenta and uterine musculature. This ratio balances the excess hormone content, ensures proper labor, and prevents too strong contractions.
The task of oxytocin during childbirth is to stimulate contraction of the uterine muscles, forcing the cervix to open. Thanks to this, delivery is ensured. In addition, the hormone oxytocin after childbirth promotes the production of colostrum and then milk.
If labor is difficult due to insufficient dilatation of the cervix, doctors use a synthetic drug - an analogue of the female hormone - to stimulate the uterus.
Rapid contraction of the uterus
Women who are cleared of the effects of childbirth within 3-4 weeks are usually happy with such a quick recovery and are proud to tell everyone about it. Few of them think about the fact that such rapidity is not the norm and can lead to the most negative consequences for health. In most cases, rapid contraction of the uterus after childbirth can be fraught with the following complications:
lochia (remnants of the placenta, blood clots, burst vessels, dead endometrium, waste products of the child when he was in the womb) cannot be released in full in such a short period of time: this means that part of all this remains inside the uterus; this most often leads to their suppuration and the onset of the inflammatory process; lactation disorders: the amount of milk produced can sharply decrease, and its composition change, which is often very unpleasant for the baby - to such an extent that he can stop breastfeeding; the risk of an instant second pregnancy increases, while the body is not yet physically ready for such a shock.
Considering these factors, you should not be happy if postpartum discharge stops very quickly. To prevent this from happening, you need to try to improve the contraction of the uterus after childbirth so that it occurs within normal limits and does not go beyond their limits. To do this, you need to follow (if possible) a daily routine, eat well, get enough rest, get enough sleep and breathe fresh air. The use of medications and folk remedies is not required here. However, there are not many such cases: the problem of too long uterine contractions is much more common.
Features of the form and methods of administration
Oxytocin is the first artificially created hormone. The mechanism for its synthesis was discovered in the twentieth century - in 1954, for which its author was awarded the Nobel Prize. Subsequent studies revealed that it not only regulates labor and lactation, but also promotes the development of maternal instinct. It was also found that oxytocin has a beneficial effect on a woman’s psycho-emotional state: it relieves anxiety, nervous excitement, restoring peace and a sense of security. To date, all the properties of the hormone and its role have not been fully disclosed, so research continues.
The synthetic product is a complete analogue of the endogenous substance. After oral administration, it is quickly destroyed by gastrointestinal enzymes, so it is used parenterally. The drug is produced in the form of a solution in ampoules containing 5 IU.
The medication is intended for injection under the skin, muscle or vein. In obstetrics, an intravenous drip is used to induce labor. This method helps to avoid an overdose, which can provoke too intense contractions of the uterus and rapid labor, which poses a great threat to the woman and child.
After intravenous administration, the effect of the drug appears within a couple of minutes and lasts for several hours. After childbirth, intravenous administration is indicated if there is a threat of uterine bleeding.
IM injections of Oxytocin after childbirth are indicated to ensure lactation.
If a woman has had a cesarean section, the injections are administered into the wall of the uterus, or, in case of minor interventions, under the skin.
How does this happen
To understand what the process of uterine contraction after childbirth is, you need to know what happens to the body during this period. Without anatomy, this issue cannot be understood.
In the first time after childbirth, the organ is a wound surface. The part of the uterus where the placenta was attached is especially damaged, because there are too many clogged vessels in that place. The cavity itself contains remnants of the membrane from the fetus and blood clots. Cleansing of the uterus and its most powerful contraction occurs during the first 3-5 days after birth. If the body is healthy, processes such as phagocytosis (leukocytes dissolve bacteria) and extracellular proteliosis (the same bacteria are attacked by proteolytic enzymes) begin to actively occur. As a result, lochia and postpartum discharge begin to appear: on the 1st day it resembles blood, on the 3rd day it acquires a serous-hysterical tint, by the end of the 3rd week it becomes light and liquid, by the 6th it should end, which will happen signify the completion of the uterine contraction process. As for the size, immediately after the birth of the baby, the uterus weighs about 1 kg, its throat expands to 12 cm. At the same time, it reaches 20 cm in length and up to 15 cm in width. After a week, its weight will be only 300 grams, and by 7th week - only 70 grams.
The epithelium of this organ is restored in about 3 weeks, but the place where the placenta was previously attached heals much longer - up to 1.5 months. It is very important to observe how long the uterine contraction lasts after childbirth in each individual case and compare the period with the standard. If the lochia ends by the 6th week and there is no discomfort, there is no need to worry: everything is normal. If they stopped much earlier or, on the contrary, still continue after this time, you should definitely complain about these symptoms to a doctor. There are special signs by which you can judge whether everything is in order with you.
Wow! The standard size of a healthy uterus in its normal state, when a woman is not pregnant, is 7.5 cm in height and 5 cm in width. However, by the time the baby is born, it is so stretched that it touches the lower part of the chest. After giving birth, she has to shrink back to her normal size.
Reasons for using the drug during childbirth
For a doctor to prescribe Oxytocin during labor, there must be a good reason. If the pregnancy developed correctly, without any complications, labor began on time and proceeds naturally, there is no need for the drug. Even if, in the opinion of the woman in labor, the process has been delayed and needs to be accelerated. To start administering a drug, you need really good reasons. Therefore, the decision to use the drug Oxytocin during childbirth is made only by a doctor for medical reasons if the following factors exist:
- Preeclampsia
- Long (more than 12 hours) period after the rupture of amniotic fluid
- Weakness of labor.
- Prevention of uterine bleeding after childbirth or after cesarean section.
- Weak contraction of the uterus. This may lead to bleeding or inflammatory diseases.
- Rhesus conflict in a woman in labor
- Post-term pregnancy
- Stillbirth.
Each of these conditions can pose not only a threat to health, but also life. Therefore, to speed up labor, a decision is made to administer Oxytocin.
Symptoms of normal contraction
Every woman needs to know the signs of good uterine contraction after childbirth, which indicate a normal recovery period without any abnormalities. This will mean that there is no need to worry and all your strength can be directed to the child. Such manifestations include:
painful but tolerable sensations in the mammary glands; discomfort in the lower abdomen; first bloody, then yellowish-transparent lochia; pain in the perineum; diarrhea during uterine contractions can be observed only in the first 1-4 days; in other cases, it may indicate an overdose of some drug and will require medical intervention; all these symptoms are quite strong in the 1st week after the birth of the baby, since uterine contractions occur most intensely during these days; by the end of the 6th week, all these signs gradually disappear.
All pain during uterine contractions after childbirth, described above, is quite tolerable, although if a woman has a low pain threshold, the doctor often prescribes painkillers. These include:
no-shpa; ibuprofen; ketoprofen (this active substance contains ketonal suppositories); You can relieve pain from uterine contractions using lidocaine injections; naproxen; homeopathic medicines: Bellis perennis, Caulophyllum, Sepia.
If after the first week the painful contractions remain as strong and even unbearable, this is a reason to seek medical help; such discomfort is not the norm. Since everyone’s body is different, gynecologists admit that for some, the recovery period can last from 5 to 8 weeks. If it goes beyond these limits, perhaps we are talking about pathologies, so it is better to get checked again.
Sometimes it happens! There were cases when women were diagnosed with 2 uteruses, each of which was a full-fledged, functioning organ. Moreover, some of them successfully gave birth to healthy babies. One of the organs was involved in the process of gestation and childbirth.
Reasons for prescribing hormones after childbirth
Oxytocin can also be prescribed after the birth of a child. After the fetus is delivered, the process of returning the uterus to its previous size and functions begins. It lasts for several months, but is especially active in the first three days after birth. At the same time, the condition of the blood vessels at the placenta insertion site is normalized.
If the process is delayed, this can lead to complications and inflammation, and then the question of administering the drug Oxytocin after childbirth is considered.
Side effects of oxytocin
Prolonged administration of oxytocin during and after childbirth can cause swelling that subsides a few days after birth. This is due to its ability to delay the outflow of urine and accumulate fluid in the body.
There may be a slight increase in blood pressure and arrhythmia with both the fast and slow route of administration, as well as nausea and vomiting.
Of course, after childbirth, your own hormones are better than synthetic ones. A good positive attitude and breastfeeding are essential to stimulate oxytocin production. But having weighed all the pros and cons of the use of its synthetic analogue by doctors after childbirth, we agree that its additional administration in the maternity hospital is necessary not to assuage the conscience of the medical staff, but for your own benefit. And painful contractions are also felt during natural contractions during breastfeeding. Health to you and the baby!
The role of the hormone in hepatitis B
The role of oxytocin during breastfeeding is no less important. The thing is that two interrelated hormones are responsible for the normal course of lactation - the release and separation of milk in the required volume: prolactin and oxytocin.
The signal for the production of the first substance is the start of the baby sucking at the breast. Most of it is produced from 3 to 7 am. The secretion of prolactin is also activated when the baby cries and expresses the breast.
But during lactation, it is important not only to produce milk in the required volume, but also to release it from the breast. And this process is controlled by oxytocin, which, in turn, depends on the emotional state of the young mother. If a woman is calm and at peace, then enough oxytocin is produced to send a signal to the mammary ducts to relax. In this case, mother's milk is released without difficulty. But if a woman is nervous, less oxytocin is produced, then the breasts are tense, the outflow of milk stops or it is not released enough.
Therefore, if a woman has difficulty feeding her baby, she may be prescribed the drug Oxytocin while breastfeeding to activate the production of prolactin.
Slow contraction of the uterus
Very often, postpartum discharge and painful sensations drag on and do not stop even after the normal 8 weeks have passed. In this case, a whole problem arises: how to speed up the contraction of the uterus after childbirth and help your own body recover faster. First, you need to contact the observing gynecologist and follow his advice. Secondly, with his permission, perform various exercises specially designed for this purpose and use folk remedies.
Health care
If in the first 1-3 days after the birth of the baby, a woman does not begin to discharge and there are no painful, cramping sensations, this indicates that for some reason the process does not start. In this case, the doctor decides what to do to contract the uterus after childbirth: give injections or prescribe pills.
Oxytocin
In order to speed up uterine contractions after childbirth, prevent severe bleeding and normalize lactation, oxytocin, an artificial hormone, is prescribed. It is administered by injection, most often by injection. But if a woman is very weak after childbirth, an IV may be prescribed, especially after a caesarean section.
Uterine oxytocics
Very often, drugs for uterine contractions from the same group of oxytocins are prescribed, but not in pure form, but with pharmacological additives that enhance and weaken the effect of the main substance. These include hyfotocin, demoxytocin, dinoprost, dinoprostone, cotarnine chloride, methyloxytocin, methylergometrine, pituitrine, ergometrine, ergotal, ergotamine hydrotartrate. These could be pills or injections.
Any medicine is prescribed only if poor uterine contractions after childbirth are diagnosed (no discharge or cramping pain in the lower abdomen). However, the attitude towards oxytocin even among doctors is ambiguous. Most of them believe that this process should start naturally. Therefore, some gynecologists recommend turning to folk remedies for help.
Folk remedies
There are also folk remedies for contracting the uterus. However, you should not get carried away with them and it is recommended to use them only with the permission of a doctor.
Nettle
Dry nettle (4 tablespoons) is brewed with boiling water (500 ml). Let it sit until it cools down. Drink 100 ml three times a day.
White lily
Pour the flowers of the plant (2 tablespoons) with cold boiled water (500 ml). Leave overnight. Strain. Drink 100 ml 3 (or 4) times a day.
Shepherd's Purse
The herb is brewed (4 tablespoons) with boiling water (2 glasses). Wrap up, leave in a warm place, strain. Drink the entire prepared dose during the day.
Yarutka field
Brew the dry plant (2 tablespoons) with boiling water (a glass), leave overnight, strain. Drink 1 teaspoon 5 times a day.
Blood red geranium
Pour 2 teaspoons of herb into 2 glasses of boiled, but cold water, leave overnight, drink everything during the day.
Folk remedies for uterine contractions are good because they force the body to actively recover during the postpartum period on its own, without the use of synthetic drugs, the effect of which on the child (through breast milk) and on the health of the young mother has not yet been fully studied.
Massage
In some cases, uterine contraction is stimulated from the inside when the doctor gives the woman a special massage every two hours in the first two days after childbirth. Smooth movements apply pressure to the uterus. Depending on the individual characteristics of the body, this procedure can be very painful, but useful.
Homeopathy
In order for the uterus to contract faster, homeopathy is used, the main advantage of which is that it mobilizes the body’s own forces and does not contain any synthetic, chemical substances.
Among the well-proven drugs, the following can be noted: Millefolium, Hina (excessive bleeding), Ergot (perfectly contracts the uterus, but can provoke the development of thrombosis, phlebitis, abscess), Sabina (distinguished by the absence of side effects), Ipecac (helps cope with weakness after childbirth ), Sekale, Phosphorus, Hamamelis, Ferrum phosphoricum, Staphysagria (promotes healing of the uterus).
Exercises
If the doctor allows it, from the first day after childbirth you can perform simple but very useful physical exercises to contract the uterus after childbirth, which will not require much effort and time from the woman. The sooner you start doing them, the lower the risk of a protracted recovery period.
Lie on the floor on your back. Relax. Bring your legs together. Bend and unbend them at a calm pace. Do 10 times. At any free time, tuck and relax your toes. Lie on the floor on your back. Relax. Straighten your legs. Pull your toes toward you as much as possible. Breathing exercises for contracting the uterus help well, which can be done several times daily. Lie on your back. Bend your legs. Breathe deeply and evenly. Connect your abdominal muscles to this process. Raise the abdominal wall as you inhale and lower it as you exhale. Help yourself with sliding movements of your hands towards the pubic bone from the navel. Exhaling, squeeze your pelvic muscles and pull your navel as close to your chest as possible. Concentrate on the sensations in your lower abdomen. Hold your breath for 10 seconds. Such exercise must necessarily include Kegel exercises: alternately strain (squeeze as much as possible) the muscles of the anus and vagina. Exercise regularly to promote postpartum uterine contractions. Prepare an exercise ball. You will need to perform the exercise on a non-slip floor. Sit on the ball, squeeze your intimate muscles. In this position, raise your leg and hold it suspended for about 10 seconds. Repeat the same movements with the second leg. Sitting on a gymnastic ball, perform circular movements with your pelvis in both directions. Sitting on the ball, swing in different directions.
Exercises for rapid contraction of the uterus after childbirth should not be performed by those who have had stitches. First you will need to wait for them to heal completely.
Side effects of the drug
The use of a synthetic hormone is associated with the risk of undesirable conditions, which manifest themselves in the form of:
- Digestive disorders
- Nausea, vomiting
- Fluid retention, swelling (occurs when IV infusion of drugs is too long)
- Disorders of the cardiovascular system in mother and fetus: abnormal heart contractions, arrhythmia, increase or sharp decrease in blood pressure, the occurrence of SAH (subarachnoid hemorrhage)
- Unbalanced or too active labor
- Intrauterine fetal suffering
- Rupture of the walls of the uterus (can lead to death of the mother in labor)
- Untimely placental abruption
- Increased tone of the uterus
- Hypersensitivity reactions (rashes, itchy skin)
- Other reactions: bronchospasms, yellowing of the skin in a newborn, a sharp drop in the concentration of the hormone fibrinogen in the fetus.
Indications
Oxytocin is multifunctional, the described actions characterize it as a necessary, important and useful substance. Nevertheless, serious consequences have been described after stimulation, the main reason for which is a gross violation of the instructions for using the hormonal drug.
There are special indications for prescribing the drug. During childbirth, administration of the drug is necessary:
- with toxicosis,
- release of amniotic fluid long before the onset of active labor,
- pathologies dangerous to the life of the mother and fetus,
- Rhesus conflict,
- absence of contractions.
Postpartum administration of the hormone is a prevention of bleeding ; the drug is necessary if the uterus contracts slowly. Correct use of the hormone allows you to avoid serious complications. For example, when a child is in the birth canal for a long time, this can cause the mother to develop fistulas in the organs of the reproductive and digestive systems, the child experiences cerebrovascular accidents, and hemorrhage in the brain can occur.
Who should not administer Oxytocin?
The drug is administered according to medical indications. Oxytocin should not be used if you have:
- Individual hypersensitivity to synthetic hormone
- Disproportion between the sizes of the mother's pelvis and the fetus's head
- Threat of uterine rupture, insufficient organ development
- Obstructions in the birth canal (tumors, spasms, scar changes)
- Fetal size is too large, hydrocephalus
- Abnormal (oblique or transverse) position of the fetus, which makes natural passage through the birth canal impossible
- Pathological presentation of the umbilical cord
- Multiple births.
Stimulation of labor with Oxytocin is, unfortunately, not uncommon these days. And often the drug is used unreasonably often. Therefore, recently, doctors and patients themselves have developed an ambiguous attitude towards the drug Oxytocin, which was previously considered safe. Unlike the natural hormone of the same name, a synthetic product, in addition to helping, can also cause harm. Therefore, the decision to include it in obstetric care should be considered especially carefully.
Contraindications
Even if the administration of oxytocin is correctly prescribed, the doctor must make sure that the woman has no contraindications to the use of the drug. They can be absolute and relative. Absolute contraindications include:
- the baby’s head does not correspond to the size of the birth canal of the woman in labor,
- malpresentation of the baby,
- natural childbirth is impossible
- threat of rupture of the uterine walls,
- the presence of scars on the walls of the uterus of various origins (caesarean section, other operations),
- neoplasms on the cervix,
- pathologies that interfere with the opening of the uterus,
- hypersensitivity to the drug,
- hyperstimulation with a hormonal agent has already been used,
- immaturity of the cervix.
Relative medical contraindications include:
- pregnancy with twins,
- diagnosed with uterine fibroids,
- the fetus has hypoxia.
If there are relative medical contraindications, stimulation should be prescribed very carefully. It is in these cases that negative consequences are observed.
Stimulation procedure
The drug is administered into the body in different ways: into a vein, under the skin, intramuscularly. You can inject oxytocin directly into the uterus. To stimulate the uterus during labor:
- An oxytocin drip is placed (intravenous infusion).
- The course of the labor pains of the woman in labor is constantly monitored, and the baby’s heartbeat is monitored.
- In the standard procedure, the hormone concentration is 1 ml (or 5 IU) per 500 ml of sodium chloride (glucose can be used as a solvent).
- The rate of administration of the drug is no more than 8 drops. Every 40 minutes, the number of drops is increased by 5 until the desired degree of myometrial contraction is achieved. Further, the concentration of the substance decreases in the reverse order.
For bleeding after childbirth use:
- dropper - per 1000 ml of solvent up to 40 IU of oxytocin,
- intramuscular injection - 1 ml (5 IU) after separation and delivery of the placenta.
Prevention of bleeding:
- 2-3 days intramuscular injections 3 times a day, 5 IU of the hormone,
- after a cesarean section, 5 IU of oxytocin is injected into the muscular wall of the uterus.
The stimulating effect of the drug begins quickly, 3-5 minutes after administration, the activity of the substance lasts up to 3 hours.