≡ Home → Cervix → Erosion →
Quite often, after the next preventive examination by a gynecologist, a woman hears the phrase: “You have cervical erosion!” And this is perhaps the most common diagnosis in women of childbearing age.
However, in fact, it turns out that in our time the concept of “erosion” is absent in professional medicine throughout the world, except for Russia. In our country, for some unknown reason, this term has taken root firmly, although today it has been precisely proven that it is absolutely incorrect and does not reflect the essence of the processes occurring on the mucous membrane of the cervix.
Is there actually erosion?
Translated from Latin, “erosio” means “corrosion.” For many years, it was believed that erosion was a defect in the cervical tissue (ulcer) that could develop into cervical cancer if not treated. And cauterization was carried out on all women in a row. This is how it was in the time of our grandmothers and mothers.
As time passed, gynecology developed progressively, and the following became clear:
- There is virtually no cervical cancer without infection with the human papillomavirus;
- The presence of erosion in itself does not increase or decrease the likelihood of developing cancer;
- Often erosion is not erosion at all, but ectopia;
- Ectopy is the migration of cervical epithelial cells from the inner part of the cervix to the outer surface;
- Ectopia is not a disease, but a physiological condition of the cervix that does not need to be treated: over time it goes away on its own.
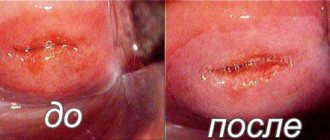
This is what large cervical erosion on the anterior and posterior lips looks like during colposcopy.
On a note
Cervical erosion is not a female disease that needs to be treated. This is the norm. In other words, cells turn from the inside out (in medical parlance, this condition may be called ectropion). No matter how paradoxical it may sound, if you do nothing about such erosion, it will go away on its own.
Therefore, if you are informed that you have been diagnosed with erosion, do not panic, do not rush to remove it and spend money on treatment, the cost of which is often quite high.
We repeat once again that the concept of erosion is outdated, and it is more correct to say ectopia (false erosion or pseudo-erosion). But this term has become so firmly established in our everyday life that it continues to be used not only by patients, but, oddly enough, even by doctors. This is probably due to a lack of information among women. If the patient is told that she has “erosion,” then no additional questions arise, because she heard this name from her friends, mother or grandmother. But if you tell a woman that she has ectopia or ectropion, then she is unlikely to immediately understand what the doctor is talking about; she will also decide that something terrible and dangerous has been discovered in her.
This is what a large cervical ectopia looks like during colposcopy.
Therefore, doctors still have a long way to go to eliminate illiteracy among the female population.
On a note
The term “erosion” is currently used exclusively for true erosions that arise as a result of an infectious process, trauma or radiation.
Briefly about the symptoms
At an early stage of development, ectopia does not manifest itself symptomatically and the woman is not aware of the development of problems. The main question asked by women to gynecologists is as follows: can the cervix hurt due to erosion? No, pain in this area is excluded, discomfort can occur with cumulative damage to nearby organs, because the cervix does not have nerve endings, which is why characteristic signs of erosion most often appear after sexual intercourse, ultrasound or gynecological examination.
The list of the most common signs that worry women with cervical erosion includes:
- Discharge with blood after sexual intercourse and painful contacts. At the initial stage, the volume of blood released is minimal. It increases significantly as the volume of erosion itself changes.
- Sharp pain in the lower abdomen after lifting weights and other physical activities. The symptom is also often accompanied by bleeding. The symptom occurs regardless of the phase of the menstrual cycle.
- Discharge of an unusual color. Erosion is a favorable environment that provides rapid development of pathogenic microorganisms. Mucus secreted from the cervix has a yellow or green tint and has a pungent odor.
- During urination, pulling or shooting pains appear in the lumbar region.
- Typical menstrual cycle disorders. Bleeding occurs several times within 1 month. The periods themselves become more abundant. Against this background, anemia progresses.
Diagnosing the lesion independently, without a gynecological examination, is possible only at an advanced stage, when all of the listed symptoms appear. The main danger is that patients often ignore the first signs of damage and consult a doctor in critical condition.
Attention! Lack of timely treatment of erosive lesions causes the formation of leukoplakia or erythroplakia.
Having examined in detail the structure of the lesion, we can say that erosion is a bleeding surface that promotes the proliferation of pathogenic microorganisms. The moist and warm environment of the vagina is ideal for such processes. Since the cervix and cervical canal are a direct path to the uterus, damage to the reproductive organ by various pathogens is possible.
Can pain occur?
Ectopia or erosion often occurs without symptoms. A woman with this pathology is able to lead a normal lifestyle without thinking about any changes. Due to the increased sensitivity of the mucous membranes, blood may be released after sexual intercourse, but in small quantities.
As pathological progress progresses, discomfort and pain appear. The reason for the appearance of noticeable discomfort is the increased activity of pathogens, namely chlamydia, mycoplasma or ureoplasma. Infection occurs through unprotected sexual intercourse if one of the partners is infected. An equally common cause of pathogen activity is non-compliance with intimate hygiene rules and decreased immunity.
Detection of any symptoms of discomfort should be the reason for a high-quality gynecological examination. It is impossible to eliminate pain without addressing its cause; the patient’s condition will worsen. If discomfort appears, the reason is secondary infection; under such conditions, the ectopia will not heal on its own. Due to a decrease in local immunity, the ability to regenerate is lost.
Characteristic discharge
Erosion is a lesion of the mucous membrane of the vaginal part of the cervix. There are a sufficient number of reasons for its appearance. If the affected area is small, there are no symptoms. The nature of the discharge changes due to the addition of infection and the production of decay products by pathogens.
Normal or natural for a woman's vagina is mucous discharge. Produced by the glands of the cervical canal. They can be white or colorless and have no foreign odor. Their consistency changes during the menstrual cycle. In the first phase they are thick and viscous, during ovulation they are abundant and more liquid, and at the end of the cycle they become thick.
A change in the shade of the discharge is the first marker of the development of the pathological process. Yellow, green or other pathological discharge indicates an infectious process occurring against the background of erosion. The background course of such diseases cannot be excluded:
- colpitis;
- vaginitis;
- vaginosis;
- gardnerellosis;
- trichomoniasis;
- adnexitis;
- salpingitis.
You shouldn't worry too much about this. Detection of changes of this nature is simply a reason for an unscheduled visit to a gynecologist. Basically, the symptom is not associated with the development of serious diseases. A indicates a violation of the vaginal microflora.
Itching and burning
Symptoms such as itching and burning in the genital area are most often not associated with erosive lesions of the cervix. Such signs are characteristic of other diseases of the reproductive system that are infectious in nature. If they appear against the background of erosion, the development of infection can be assumed.
In this case, the treatment regimen is supplemented with anti-inflammatory and antibacterial drugs. Most often, topical agents are used: suppositories, ointments, antiseptic sprays. After them, the affected area stops aching and itching, and swelling is eliminated. A burning sensation when affected by erosion does not appear; this symptom is characteristic of infectious processes.
How is the cervix structured?
To clearly understand what we are talking about, you need to have minimal knowledge of anatomy and know how the organ we are talking about works.
So, that part of the cervix that is located in the vagina and which the doctor sees during a gynecological examination in the speculum is quite logically called the vaginal part of the cervix. Inside the cervix is the cervical, or cervical, canal, which opens into the uterine cavity. There are two physiological narrowings in the cervical canal - the external and internal pharynx. The external os opens into the vagina. In nulliparous women, it is round in shape, and after childbirth it takes on the appearance of a transverse slit. The internal os opens into the uterine cavity. The cervical canal contains mucus, the main function of which is to prevent infection from entering the uterine cavity from the vagina.
The structure of the cervix.
The outside of the vaginal part of the cervix is covered by stratified squamous epithelium. The word “multilayered” itself suggests that it consists of several layers of cells. Thus, it has a significant (of course, by microscopic standards) thickness and performs a protective function. The mucous membrane of the cervix, covered with stratified epithelium, has a pale pink color.
Inside the cervical canal there is a cylindrical, or glandular, epithelium. It is thinner and more delicate, consists of a single row of cells, and the blood vessels shining through it give it a red color.
The columnar epithelium has a completely different function - to produce mucus. Columnar epithelium is hormone-dependent: when there are a lot of female sex hormones, it produces liquid mucus, when there is little, thick mucus. This invention was invented by nature for conception: through liquid mucus, sperm very easily penetrate the uterine cavity, meet the egg, and fertilization occurs. This quality of mucus is observed during the period of ovulation. The rest of the time, cervical mucus is thick, viscous, its function is protective - no infectious agent can penetrate the uterine cavity and cause inflammation.
The zone where two types of epithelium meet is called the transition zone, or transformation zone. At different age periods of a woman, this zone is located at different levels, which depends on the stage of development of the female reproductive system.
Thus, in newborn girls and virgins, the junction zone is located on the outer cervical surface. In this case, they talk about congenital erosion.
Histological structure of different types of cervical epithelium (in women of reproductive age and during menopause).
During puberty or during pregnancy, when a high level of sex hormones is noted in the female body, the cylindrical epithelium begins to quickly “crawl” out of the cervical canal and is located around the external pharynx, resulting in the formation of a red spot in this place. The same can happen if a woman takes hormonal contraceptives.
As a girl grows up, the level of sex hormones decreases, the stratified squamous epithelium begins to displace the cylindrical epithelium into its place - into the cervical canal, and the junction zone moves closer to the external pharynx.
With age, the border of the two epithelia completely hides deep into the cervical canal, which is why it becomes invisible. Therefore, ectopia no longer occurs in women of the older age group.
It is also useful to read: What discharge is considered normal for cervical erosion?
Reasons for the development of the disease
The cause of erosion is sometimes quite easy to determine. The main prerequisite is considered to be changes in hormonal levels that occur during puberty, with deviations in delivery or diseases of the endocrine system. The following may act as provoking factors:
- inflammatory in nature - suggests the presence of a pathogenic agent, for example, bacteria or fungal infection. There is also a special condition - ectropion, when the cervical canal is inverted into the vagina, and inflammation is also present;
- changes in hormonal levels that occurred during a certain period or during a systemic disease;
- injuries received during manipulation, sexual intercourse, surgery;
- the consequences of using certain medications, for example, birth control pills, which have a suppressive effect on natural processes in the body.
The causes of this pathological phenomenon, that is, inflammation, which led to the destruction of epithelial cells in a separate area of the cervix, determine the differentiation of erosion into true or pseudo . If there is no violation of tissue integrity, then we are talking about pseudo-erosion. In cases in which there is damage to the epithelial layer, a diagnosis of “true erosion” is made. The treatment tactics are usually chosen by the doctor depending on the conclusion. Sometimes the patient remains under medical supervision, but treatment is not carried out if there is no growth and development of the negative process.
Let's take a look at the medical history...
So, we have already mentioned that ectopia (we will get used to speaking correctly) is a common condition in which a gynecologist sees a red spot around the external os of the cervix. Previously, due to imperfect research methods, it was believed that this was a defect in the cervical tissue, which could turn into cancer if left untreated. Therefore, in order to prevent cervical cancer, they tried to eliminate this defect by cauterization. Moreover, cauterization was performed on almost all women in 100% of cases.
But science moved forward. It became clear that the doctor’s eye cannot examine the cervix and its defect in detail: after all, it is necessary to evaluate the quality and structure of the cells. But it is almost impossible to do this with the naked eye. And in the daily practice of gynecologists, colposcopes began to appear - microscopes for a detailed study of the condition of the cervix.
The procedure of colposcopy, examination of the cervix in mirrors under microscope magnification, allows you to assess the condition of the epithelium and the presence of pathological changes.
Diagnostics have become more advanced. It was established that “erosion” is not an area devoid of epithelium at all, but a displacement of the intracervical columnar epithelium onto the vaginal part of the cervix. It is the columnar epithelium on the surface of the cervix that looks like a red spot.
Why the pain starts, reasons
The causes of true or false erosion vary.
This disease is caused by bacteria or fungi (chlamydia, ureaplasma, mycoplasma).
They are transmitted from a partner or appear due to improper hygiene or weakened immunity.
Irregularity of menstruation should also alert a woman. This may be a signal of an inflammatory process or hormonal imbalance, which can cause disturbances in the mucous membrane of the cervical canal.
An insufficient amount of female sex hormones worsens the condition of the cervix. It becomes loose and easily susceptible to infection or damage.
Early sexual activity has a negative impact on women's health, exposing a young and unprepared body to infections or diseases.
This pathology of the female reproductive system does not have a pronounced pain syndrome at an early stage .
But everything in the body is interconnected, therefore, at an advanced stage of the disease, it is accompanied by serious problems or pain.
Under the influence of bacteria, you can additionally get cystitis, endometritis, salpingitis, and colpitis.
In case of hormonal imbalance, menstruation is profuse and painful.
Mechanical damage to the cervix causes discomfort during sexual intercourse and bleeding.
Types of erosion
Experts distinguish the following types of cervical erosion:
- Ectopia, or pseudo-erosion (sometimes in the scientific literature you can find the name “false erosion”). It occurs when the internal epithelium of the cervical canal shifts to the surface of the cervix (this was discussed above);
- True erosion. We can talk about it when a defect appears on the outer part of the cervix and the stratified squamous epithelium is completely absent. The reason for this may be an inflammatory process, trauma to the cervix with gynecological instruments, or constant trauma to it due to uterine prolapse.
On a note
In young women, true erosion is extremely rare, while ectopia is quite common. On the contrary, in women over 40 years of age, ectopia is an extremely rare phenomenon. For this age, true erosions are more typical.
This is what pseudo-erosion and true erosion of the cervix look like during colposcopy.
What is the nature of pain against the background of erosion?
Often, periodic or constant pain in the lower abdomen is associated with the menstrual cycle, but pain can appear regardless of the menstrual days. It is imperative to pay attention to the connection with urination: with cystitis and urethritis, pain occurs when visiting the toilet. Possible options for pain in the lower abdomen:
- pulling,
- pressing,
- aching,
- stabbing,
- cutting.
Against the background of inflammation in the ovaries and uterus, hormonal problems may arise, which will be manifested by the following changes:
- the menstrual cycle is disrupted (untimely arrival of menstruation, heavy or scanty periods, pain in the first days of menstruation);
- breasts swell and hurt;
- there is no desired pregnancy.
When a woman undergoes examination and treatment for erosion on the cervical surface, it is necessary to promptly inform the doctor about all changes associated with the regularity of the menstrual cycle or any atypical symptoms.
These problems are caused by hormonal imbalances that need to be identified and treated.
How is ectopia diagnosed?
There is no diagnosis of cervical erosion worldwide. However, although today most practitioners do not consider cervical erosion a disease and claim that there is no such diagnosis, in the international classification of diseases of the 10th revision (ICD-10) under the heading “Non-inflammatory diseases of the female genital organs” it is assigned code N86. Allow me a small clarification: this section refers only to a case of ectopia with complications, that is, a pathology variant that requires treatment.
Ectopia is a condition that has no symptoms. And only a gynecologist can detect it during an examination. Very rarely (when the ectopia reaches a large size), there may be complaints of spotting after intimacy, or copious white or mucous discharge from the vagina may appear. There is never pain during erosion. And it cannot be seen on an ultrasound.
So, what does a doctor do if he discovers an unclear red spot on the patient’s cervix during a gynecological examination?
Firstly, the doctor will definitely take smears from the cervix for atypical cells. A smear for cancer cells in gynecology is called a Pap test. This is a very important analysis. Even if a woman is gynecologically healthy, she must undergo it without fail once a year.
The process of collecting material for a Pap test.
On a note
Cervical Papanicolaou smear examination (PAP test) is the main method for identifying precancerous conditions of the cervix. Material for cytology is collected from three areas: from the outer part of the cervix, from the junction of stratified squamous and columnar epithelium, and from the lower third of the cervical canal. To take material for examination, special brushes are used.
Heal with medicinal herbs
Healing herbs are effectively used to treat diseases at home.
Application of bergenia extract
This plant is characterized by anti-inflammatory and antimicrobial effects. In addition, bergenia has antitumor, hemostatic and vasoconstrictor effects. It is used to cure fibroids, inflammation of the appendages and cysts.
Extract preparation:
- Grind the root of the plant.
- Pour 3 tbsp of water into a glass. spoons of the resulting product.
- Gradually evaporate the mixture until it is reduced by half.
- The extract is filtered while hot.
Before the douching procedure, you need to dilute 1-2 tbsp. spoons of healing extract with 0.5 liters of warm liquid.
Use of Kirkazon and Celandine
These plants are effectively used to cure erosion, as well as fibroids and endometriosis. To make an infusion, mix 3 tbsp. spoons of Kirkazon with 1 tbsp. spoon of celandine. The mixture should be poured with a liter of boiling water. Let the infusion cool and then strain.
The healing infusion is used for douching. Duration of therapy is 10 days. After a break, treatment with infusion can be repeated.
The use of St. John's wort infusion
We treat erosion by douching with St. John's wort infusion. To make the latter, pour 4 tbsp. spoons of raw materials 2 liters of hot water. Boil over low heat for 10 minutes, and then let it brew for half an hour. Douche several times a day.
Resin therapy
An ointment is prepared to treat the disease. To prepare the latter, you need to melt the butter in an enamel container, skimming off the foam. Drain off the clean oil and discard the remaining oil. 200 ml of ghee must be mixed with natural wax, as well as crushed resin in an amount of 2 boxes of matches. The mixture should be heated, but not higher than 800 C. When all the ingredients have dissolved, strain the mixture. As the mass begins to thicken, add 1 teaspoon of honey. The mixture is thoroughly mixed. To heal with this ointment, lubricate tampons.
Important! The medicinal ointment must be stored in the freezer.
Treatment of Kalanchoe
The juice is squeezed out of the plant, which is mixed in equal parts with honey and sunflower oil. The product is boiled and allowed to cool. Leave to infuse for a week. Mix the mixture thoroughly before use. Heat some of the product and soak the tampon in it. In the mornings, it is recommended to douche with chamomile infusion.
The duration of such treatment will be 10 days.
Eucalyptus infusion
To prepare a healing infusion, you need to pour 0.5 liters of boiling water with 2 tbsp. spoons of eucalyptus and boil for 5 minutes over low heat. Let it brew. It is recommended to use the resulting infusion for daily douching in the evening. To do this, in a lying position, a medicinal solution should be injected into the vagina. After 20 minutes, rise and the liquid flows out on its own.
To get effective results, it is recommended to insert honey tampons at night. The duration of eucalyptus therapy is 10 days. After 10 days you need to take a break for a week, and then you can repeat the course of treatment.
Uses of plantain
Tampons are made from plantain: several leaves are rolled into a tube and wrapped in gauze. Treatment procedures are carried out at night. The duration of therapy with psyllium tampons is about a month.
In addition, to prepare tampons, you can grind 5 leaves of the plant in a meat grinder and wrap them in a tampon.
Interpretation of the results of cytological examination
| Options | Cytological picture |
| 1 | Normal structure of stratified squamous epithelial cells |
| 2 | The structure of cells is changed due to the inflammatory process in the vagina and (or) cervix |
| 3 | Single atypical cells with nuclear anomalies appear, and malignancy is suspected |
| 4 | There are individual cells with obvious signs of a malignant process |
| 5 | A large number of cancer cells |
Secondly, he will take a vaginal smear for flora. The smear may contain elevated leukocytes and pathogenic microflora, which indicates inflammation of the vagina. The inflammatory process in the vagina makes it difficult to identify atypical cells, therefore, if one is detected, then it is necessary to treat it, and then repeat the cytological examination.
For sanitation of vaginal inflammation, topical preparations in suppositories or vaginal tablets are used: Terzhinan, Hexicon and others. In some cases, it may be necessary to prescribe antibiotics, and to treat thrush - antifungal agents. The doctor will select all medications taking into account the causative agent of the disease.
To speed up the healing of erosion, all existing inflammatory diseases in the vagina should be cured, as they can affect the development of the focus of an existing pathological area.
It's important to understand
All of these medications are not used to treat erosion. The purpose of their purpose is to sanitize the vagina so that microbial agents do not provoke the transition of an uncomplicated form of erosion, which does not need to be treated, into a complicated one. Complicated erosion has a less favorable prognosis and always requires therapy.
Thirdly, if a cervical defect is detected, the gynecologist will suggest taking an HPV (human papillomavirus) test. Cervical pathology is usually caused by two oncogenic types of HPV - 16 and 18.
And finally, a colposcopic examination. The doctor will examine the cervix in detail under a microscope and evaluate the structure of the cells of the spot seen, the nature of the surface, color, edges of the affected area, and vascular pattern. Colposcopy complements cytological examination and makes it possible to identify a group of healthy women - those who do not require treatment for ectopia. The purpose of this study is to identify the lesion and substantiate the indications for targeted biopsy of the cervix. There is no need to be afraid of this procedure - it is absolutely painless.
A cytology smear allows you to determine the presence of cervical diseases and identify the risk of neoplasms.
Erosion that does not go away (in which cases should you not hope for self-healing)
Pathology does not always disappear on its own without specific therapy. In certain situations, you should not rely on changes in hormonal levels. Treatment for infections does not help either. The inflammatory process in the vagina subsides, but erosion still remains or even increases in size. This phenomenon requires mandatory consultation with a doctor and additional examination.
After difficult childbirth, late abortions, or other gynecological procedures, cervical inversion may occur. During childbirth, ectropion usually forms after bilateral lateral ruptures of the neck and its subsequent suturing.
Often after childbirth, inversion of the mucous membrane of the cervix occurs - ectropion, which can only be eliminated surgically.
Externally, the formation is similar to ectopia and, in fact, also represents a displacement of the columnar epithelium. It is asymptomatic. When combined with cervicitis, it is accompanied by the appearance of pathological discharge.
Ectropion is the same erosion after childbirth that never goes away on its own. The only way to get rid of the defect is through surgery. For small lesions, laser and radio wave coagulation, argon plasma ablation and other methods are used. With severe erosion, conization of the cervix is indicated. If erosion is combined with rough scars and organ deformation, reconstructive surgery is performed.
Dysplasia, CIN (cervical intraepithelial neoplasia) are all names for the same pathology. The disease is disguised as ordinary erosion and is often asymptomatic. The disease can be recognized by colposcopy. A smear must be taken for oncocytology - an analysis that allows you to evaluate the cellular composition of the erosion. According to indications, a biopsy and histological analysis of the mucous membrane is performed.
On a note
In most cases, dysplasia occurs due to infection with HPV - the human papillomavirus.
CIN is an erosion that does not go away on its own. In the initial stages, anti-inflammatory therapy is used. As the process progresses, destructive methods of influence are indicated. CIN is considered a precancerous condition and, if left untreated, can develop into a malignant tumor.
It is also useful to read: Important aspects of treating cervical erosion in nulliparous patients
Without a doubt, cancer does not go away on its own and does not disappear under the influence of any anti-inflammatory drugs. The cancerous tumor is disguised as ordinary erosion, is asymptomatic for a long time and is often detected in late stages. Colposcopy with mandatory biopsy helps to recognize a dangerous disease. Treatment is surgical only.
Dysplasia (or CIN) may not outwardly differ from ordinary erosion, but it is considered a precancerous condition and requires mandatory treatment.
Ectopia – is it dangerous or not?
Today, medicine has firmly established that ectopia, especially small ones, is a natural stage in the development of the female reproductive system. The spot of columnar epithelium at different periods of life against the background of hormonal surges can either appear or disappear, sometimes be very small, sometimes more extensive. And with age, the body completely eliminates this area, moving the transformation zone deeper into the cervical canal.
Quite often , ectopia occurs in young nulliparous women, and is a physiological condition that does not require treatment and does not pose a health hazard.
Need to know
If you have been diagnosed with ectopia of the cervix, but a cytological examination does not reveal pathological cells and there is no human papillomavirus, then your erosion is not dangerous, nothing needs to be done about it, it will go away on its own over time. The only thing that should not be ignored is annual gynecological examinations.
If HPV is still detected, and there are no atypical cells in the Pap test, then nothing needs to be done about your erosion. Just see a gynecologist twice as often (every six months).
How dangerous is the condition?
False erosion does not pose any danger to women's health. Inflammation accompanying true erosion leads to endometritis, and in advanced forms to the development of sepsis or peritonitis.
There are cases of infection spreading to the ovaries and bladder. Suffering lymph nodes lead to painful urination and inflammation of other pelvic organs.
Lack of proper treatment can manifest itself in the form of polyps or polycystic ovaries, cervix.
The tumor can be benign or malignant. If there are no inflammatory processes or infectious lesions, the erosion heals itself.
Ectopia in young girls usually goes away after the first birth.
The process of restoration of the uterus, regeneration of the epithelium completely heals all cracks and ulcers. Don't worry if you notice erosion.
In almost all cases, it can be treated; the main thing is to choose a method that is acceptable to you. Modern medicine quickly and painlessly copes with this problem .
Drug treatment is prescribed for a period of 2 weeks to 2 months, and the rehabilitation period after surgery does not exceed a month.
When should erosion be treated?
In most cases, erosion does not need to be treated. But for this there are two conditions that should be remembered:
- There should be no inflammatory process;
- There should be no atypical or cancer cells in the smear for oncocytology.
When we talk about ectopia, we mean that the cylindrical epithelium of the cervical canal is not in its place, that is, not inside the cervix, but outside - on its vaginal part. The columnar epithelium is very thin and easily injured. The vaginal environment is not entirely natural for him. In addition, microbes can enter the vagina during sexual intercourse or from the rectum and harm the delicate epithelium.
Therefore, to prevent ectopia from developing into a complicated form, you need to keep the vagina clean, follow the rules of intimate hygiene and use condoms or spermicides during sex. This is especially true for women who are in sexual search and do not have a permanent sexual partner.
Chronic cervicitis during colposcopy (presence of hyperemia and discharge from the cervical canal).
What should I do if my Pap test reveals cancer cells?
If cancer cells are found in a cytological study, then this condition will no longer be called erosion. This is dysplasia (precancer) or even cervical cancer. In this case, you need to take a targeted biopsy from the suspicious area under the control of a colposcope.
The biopsy results are sent to the laboratory for histological examination, and only a histologist can make a final verdict, based on which the following actions are taken:
- If, according to the results of the biopsy, there is no cervical cancer, but a precancerous process is confirmed, then in this case treatment is indicated (most often by cauterization of the cervix);
- If cancer is confirmed, then the method of choice is wide conization - excision of the cervix, in which the focus of the affected tissue is removed in the form of a cone with an apex extending deep into the cervical canal.
Which cauterization method is preferable for cervical dysplasia and cancer?
Often, mild dysplasia detected may simply be a consequence of inflammation. And after anti-inflammatory therapy at the control oncocytology, not a trace will remain of it.
But if dysplasia really needs to be treated, it is important to choose the right cauterization method. When a doctor decides on the method of surgical treatment of dysplasia, the key factors are the following:
- Severity of dysplasia;
- Woman's age;
- Does her plans include motherhood in the future?
Of course, gentle surgical methods are indicated for young women with mild to moderate dysplasia who are planning to give birth after cervical treatment. For this, cauterization with laser, radio waves, argon or freezing with liquid nitrogen can be used. In case of deep lesions of the cervix in women who do not plan to give birth, diathermoelectrocoagulation or electroexcision may be justified.
Extent of spread of cervical cancer.
With advanced forms of cancer, it happens that it is not possible to save the cervix, and due to the deep germination of the tumor process, it is necessary to completely remove not only the cervix, but also the body of the uterus.
Treatment
Treatment of true erosion is carried out in two ways:
Drug therapy is prescribed in the first stages of the disease (the affected area is no more than 2 cm). In this case, concomitant diseases and the forms of their course are taken into account.
Gynecologists for vaginitis or inflammation prescribe antimicrobial suppositories: Terzhinan, Hexicon, Genferon .
For internal counteraction to infections, it is recommended to use “Metronidazole”, “Tsiprolet”, “Trichopol” . In case of hormonal imbalance, therapy is carried out based on eliminating estrogen deficiency and reducing progesterone.
Surgical intervention is carried out using the following methods:
- Cryotherapy: cauterization of the lesion with liquid nitrogen.
- Laser treatment: there is no scar on the cervix.
- Radio wave method: prescribed to nulliparous girls; after therapy there is no scar left. It is the most effective, expensive and painless.
- Electric current: after the procedure, sexual rest is required for two weeks; it is better to abstain from pregnancy for a year.
Frequently asked questions for women with cervical erosion (ectopia)
Is it possible to install a spiral if there is erosion?
Can. But only on the condition that there are no signs of inflammation in microflora smears, and there are no atypical cells in oncocytology smears.
It is important to know
Uncomplicated cervical erosion is not a contraindication for the installation of an intrauterine device.
Is it possible to have sex if there is erosion?
Can. But you need to remember that small erosion does not give any symptoms and does not interfere with sexual activity, but large ectopia (more than 1-1.5 cm) can cause bleeding after sexual intercourse. In this case, you will need to see a doctor for examination.
Is it possible to use tampons for cervical erosion?
Yes, you can.
Can erosion affect the conception of a child and the pregnancy in the future?
Erosion itself does not affect conception and does not cause obstetric complications. The problem is different. It happens that the tactics for managing and treating erosion are chosen incorrectly. An unjustified desire to cauterize uncomplicated ectopia can lead to narrowing of the cervical canal, which often causes infertility.
Why does menstruation delay due to erosion?
Cervical erosion does not affect the menstrual cycle, and delayed menstruation is associated with concomitant pathology.
What are the psychosomatic causes of erosion?
According to the theory of psychosomatics, erosion occurs in women who do not accept their feminine essence, are dissatisfied with their relationship with their partner, and experience certain difficulties in their sexual life. Official medicine does not focus on psychosomatics, so a practicing gynecologist is unlikely to recommend that his patient accept herself as a woman in terms of treating erosion (although this is exactly the advice that is given on numerous forums).
We think that from the above you understand: it is very important to decide whether your erosion is normal or pathological. The tactics of further management and treatment will depend on this. Knowing in which cases ectopia can be observed and in which it needs to be treated, you will not part with “your blood” in vain, because the cauterization offered in many clinics is paid, and the price for services is far from symbolic.
Useful video about cervical erosion
Honey therapy
The disease can be treated with honey. It is recommended to carry out the procedures every other day, and in the mornings it is necessary to douche with calendula infusion. The duration of honey therapy is 20 days.
Application of honey tampons
To prepare, fold the gauze into 3 layers, put 1 teaspoon of honey in the middle and form a tampon. The treatment procedure is carried out at night.
Therapy with honey mixture and onions
The onion must be baked in the oven. When it becomes soft, grate it on a fine grater. The resulting gruel, in the amount of 1 teaspoon, is mixed with 1 teaspoon of honey. A tampon is made from the mixture. The latter is administered at night.
For therapy, you can also take raw onions, which are grated and mixed in equal quantities with honey.
Using honey with aloe juice
To prepare a mixture for tampons, mix 2 tsp. aloe juice, 1.5 tsp. honey and 1/5 tsp. castor oil. To cure, tampons are inserted overnight.
Important! Treatment with honey is contraindicated for patients who are allergic to bee products.