Modern features of bacterial vaginosis - is it all that simple?
Bacterial vaginosis is considered a synergistic polymicrobial syndrome, which is characterized by a decrease in the concentration or complete absence of Lactobacillus SPP, mainly peroxide-producing ones, and intensive growth of obligate and facultative anaerobic opportunistic microorganisms (100-1000 times higher than normal levels). This disease has relatively recently been identified as an independent nosological form. According to modern concepts, it is defined as a dysbiotic state of the vaginal biotope.
The frequency of occurrence cannot be determined
Bacterial vaginosis (BV) is one of the most common diseases of the female genital organs. But it is not possible to determine the true incidence of BV due to the fact that it is not statistically registered, and because in 1/2 of women this disease is asymptomatic.
At the same time, in outpatient gynecological practice, BV is found in 15-19% of patients, among pregnant women it occurs in 10-30% of cases, in women with PID - in 35%.
Recently, much attention has been paid to the microecology of the genitourinary system, which contains about 10% of the microflora of a healthy woman.
Normal vaginal contents include various anaerobic or aerobic gram-positive and gram-negative microorganisms, the total titer of which is 108-1012 CFU/ml.
Among them, facultative anaerobic bacteria are found in a concentration of 103-105 CFU/ml, while anaerobic bacteria are found in a concentration of 105-109 CFU/ml.
An important component of the vaginal indigenous flora are lactobacilli, bifidobacteria and propionic acid bacteria.
The evolution of the vaginal biotope has led to the development of adaptation mechanisms that allow these microorganisms to actively develop in the vaginal environment and adhere to the epithelium, forming strong symbiotic connections with it and successfully compete with facultative and transient microflora.
The main place belongs to lactobacilli
The main place among indigenous vaginal bacteria is occupied by the genus Lactobacillus. Among lactobacilli, the most commonly isolated are L. fermentum, L. acidophilus, L. casei, L. plantarum, L. brevis, L. Jensenss.
Due to the ability to actively multiply in the vaginal environment, adhere to the surface of epithelial cells, ferment glycogen with the accumulation of organic acids, synthesize hydrogen peroxide, lysozyme, bacteriocins, stimulate local immunity, lactobacilli are most adapted to colonize the vagina and protect it from colonization by opportunistic microorganisms. This is evidenced by their high concentration in the vaginal secretions of healthy women (up to 109 CFU/ml).
In the vaginal ecosystem, the most common bifidobacteria are B. bifidum, B. longum, B. infantis, B. breve, B. adolescentis.
Vaginal bifidobacteria, like lactobacilli, are able to ferment glycogen with the formation of organic acids, adhere to the surface of the epithelium, synthesize antimicrobial metabolites, and stimulate local immunity.
They effectively suppress the growth of gardnerella, staphylococcus, escherichia, klebsiella, fungi and other opportunistic microorganisms.
In healthy women, bifidobacteria are contained in lower concentrations than lactobacilli (up to 107 CFU/ml), however, during pregnancy and especially in the prenatal period, their population level increases sharply as a powerful factor in protecting the newborn’s body from colonization by potential pathogens.
Vaginal lactobacilli are capable of synthesizing hydrogen peroxide, which suppresses the growth of obligate anaerobes of the genera Mobiluncus, Bacteroides, Peptococcus, Peptostreptococcus, Clostridium, etc. An important protective factor of the vaginal indigenous microflora is its ability to synthesize lysozyme and bacteriocins.
The colonization properties of indigenous flora depend to the greatest extent on its adhesive properties.
Attachment to the surface of epithelial cells and the formation of a biofilm on the vaginal mucosa, consisting of vaginal mucus, colonies of indigenous microflora and its metabolites, are powerful protective factors that prevent the adhesion and excessive development of opportunistic microorganisms, as well as the penetration of their cells and metabolic products beyond the vaginal tract. biotope.
Bacterial communities form biofilms
Not only indigenous microflora, but also almost all bacteria and single-celled fungi in the human body, when reproducing, form communities protected from the environment by additional membranes.
All described types of communities have a number of common properties, the main of which can be considered the isolation of the community by a shell containing an extracellular membrane and the accumulation of an extracellular matrix.
In such communities, bacteria exhibit differentiation of characteristics, as a result of which they are in different states. At the same time, a significant part has reduced metabolic activity.
Microbes within communities come into contact with each other in different planes and have a minimal free surface for contact with the matrix. Many microcolonies and similar isolated communities are united using a special matrix into a common structure called a biofilm.
Biofilm provides the bacteria within them with a significant increase in survival rate in the presence of aggressive substances and antimicrobial drugs, which must be taken into account and known in determining the tactics of management and treatment of patients.
Moreover, the result of the formation of communities and biofilms is the survival of bacteria and fungi in the presence of antibiotics in quantities 500-1000 times greater than the overwhelming concentration of drugs, which in modern conditions is taken into account when developing drugs.
Bacteriological laboratories in various countries are already beginning to evaluate antibiotics not only by the effectiveness of their action on isolated microorganisms, but also on those contained in biofilms.
With the pathological development of pathogenic microorganisms, the formation of various biofilms also occurs. Bacteria from this film are periodically released and migrate, contributing to the spread of infection, causing a deterioration in the patient's condition.
Microorganisms in communities are practically inaccessible to immune defense factors of both cells and antibodies. The use of antibiotics in regular and even increased doses turns out to be insufficient or ineffective, since the drugs do not penetrate into the biofilm in concentrations capable of coping with the microorganisms found in it.
A new look at the problem
The advent of nucleic acid amplification methods (NAAT) has allowed a new look at the problem of BV, since it has become possible to identify microorganisms that are very difficult to cultivate.
Advances in molecular biology associated with the development of the PCR method have provided new opportunities in the study of human microflora.
In addition to the qualitative identification of STI pathogens, an accurate quantitative assessment of the microflora has become possible.
This method allowed a group of authors (Collins, Wallbanks (1992)) to describe the genus Atopobium for the first time. Atopobium vaginae was first described in 1999 by Rodriguez et al., who discovered it in a vaginal tampon.
Atopobium vaginae belongs to the family Corinobacteriaceae, has a pronounced polymorphism of bacteria and is a gram-positive anaerobic rod or, according to some authors, gram-positive cocci (Schwiertz A. et al., 2006). It can occur alone, in pairs or in short chains.
Atopobium releases various organic acids during metabolism (lactic, acetic, formic, butyric, which gives a specific odor in BV).
Many authors associate the development of bacterial vaginosis and pelvic inflammatory disease (PID) with Atopobium vaginae, believing that the infection caused by it is more specific for bacterial vaginosis than the infection caused by Gardnerella vaginalis.
Highly specific marker of vaginosis
A.vaginae is considered a highly specific marker of bacterial vaginosis. Its detection indicates that a woman has this disease, which is especially important for diagnosing the asymptomatic form of BV. Atopobium vaginae, being involved in the pathogenesis of bacterial vaginosis, complicates its course and treatment.
Australian scientists (Bradshaw CS, Tabrizi SN, Fairley CK et al., 2006) showed that the presence of G. vaginalis and A. vaginae is a highly sensitive sign of bacterial vaginosis - 96 and 99%, respectively. The study involved 358 women with clinical manifestations of BV. A.
vaginae (77%) was a more specific microorganism for BV compared to G. vaginalis (35%). In recurrent bacterial vaginosis, G. vaginalis was found in 75% of cases and A. vaginae in 100% of cases. In addition, in the treatment of BV, a feature of A.
vaginae, which manifests itself in the form of high resistance to metronidazole, a traditional remedy for the treatment of bacterial vaginosis.
A. vaginae was rarely detected without G. vaginalis, and those patients in whom both microorganisms were detected had a higher relapse rate (83%) compared to patients infected with G. vaginalis only (38%, p95%), and also has an extremely safe toxicological profile.
Nifuratel does not cause teratogenic effects, so it can be used during pregnancy. A comparison between different clinical studies confirmed that, in contrast to metronidazole, there was high compliance with nifuratel treatment.
The drug demonstrates an extremely favorable risk/benefit ratio in the treatment of patients not only with BV, but also with mixed urogenital infections.
Bacterial vaginosis is one of the most common diseases of the female genital organs. But it is not possible to determine the true incidence of BV due to the fact that it is not statistically registered, and because in 1/2 of women this disease is asymptomatic.
Standard therapy for BV, adopted by Russian dermatologists in 2003, needs to be revised. Metronidazole is not the drug of choice, especially for BV associated with A. vaginae. The combination of nifuratel with nystatin turned out to be more effective both against BV and against candidiasis that often accompanies it.
The importance of nifuratel in modern gynecological practice is increasing due to its pronounced antifungal properties, since the prevalence of candidal superinfection after treatment with metronidazole or clindamycin is constantly increasing.
Source: https://medvestnik.ru/content/news/sovremennye_osobennosti_bakterialnogo_vaginoza_tak_li_vse_prosto.html
Degrees of vaginal cleanliness
https://youtu.be/6MoRVR3DpQA
Often the doctor writes out a referral for a smear test for purity. Using this method, the “degree of cleanliness” of the vagina is determined. There are four of them in total. Only the first and second degrees are normal; the third and fourth degrees indicate the presence of diseases of the genital tract.
READ MORE: Suppositories with sea buckthorn oil in gynecology. Price, names of drugs, what they are prescribed for, properties
1st degree is an ideal option, which, unfortunately, is rare. Leukocytes in the smear do not exceed the permissible limits. The flora is represented by a large number of Dederlein bacilli, mucus and desquamated epithelial cells in small quantities.
Grade 2 - The most common variant of the norm, in which leukocytes are within normal limits, mucus and epithelium are in moderate quantities. A small number of cocci or Candida fungi appear, and large quantities of lactobacilli appear.
Grade 3 - a large amount of mucus and epithelial cells is detected in the smear. There are few beneficial lactobacilli; instead, there is an increased number of Candida fungi and pathogenic microbes.
4th degree – there are so many leukocytes that the doctor describes them as “entirely”. A very large number of pathogenic microorganisms. Dederlein rods are missing. Mucus and epithelium in large quantities.
The first and second degrees do not require treatment, but the last two degrees indicate an inflammatory process caused by one or another pathogen and require immediate treatment.
Aerobic vaginitis
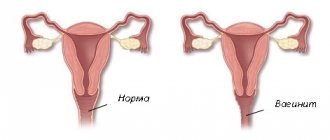
Aerobic vaginitis is vaginosis (inflammation of the vaginal mucosa), characterized by the presence of a large amount of aerobic microflora. It completely or only partially suppresses the number of beneficial lactobacilli.
Aerobic vaginitis does not pose a particular threat to a woman’s life. But it is important to remember that an advanced pathological process can provoke the development of serious complications that require long-term and specific treatment.
Bacterial vaginosis is a pathological process in the formation of which a key role is played by harmful microorganisms that multiply in the presence of access to oxygen.
Aerobic vaginitis is caused by microorganisms that thrive in the absence of oxygen.
The basis for the occurrence of inflammation in the mucous membranes of the vagina is the replacement of normal microflora by pathogenic microorganisms.
Aerobic vaginitis is provoked by factors such as a sharp decrease in the number of necessary beneficial lactobacilli, and the colonization of the mucous membranes by various pathogens. Some of them are part of the normal microflora and are opportunistic. When immunity decreases, pathogens begin to develop their activity.
Today, specialists in the field of gynecology and obstetrics cannot give an exact answer why in some cases oxygen-dependent bacteria become the cause of the development of vaginosis, and in some cases vice versa.
Causes
Viginosis of the aerobic type develops in women during the reproductive period, against the background of a general sharp decrease in the number of beneficial lactic bacteria in the vagina and their replacement with pathogenic ones.
Aerobic vaginitis is diagnosed in the vast majority of cases in girls aged 18-25 years and in women from 45 to 60 years old.
This is due to the onset of sexual activity in youth and menopausal syndrome in old age.
All these processes are marked by hormonal imbalances and surges, which in turn reduces immune defense and causes the development of genitourinary diseases.
The bacteria that most often provoke the development of aerobic vaginitis are:
- Streptococcus;
- Staphylococcus;
- Escherichia coli.
Under normal conditions, the above microorganisms are part of the normal microflora of the vagina and large intestine. If the rules of personal hygiene are violated or in the case of anal-vaginal sexual contact, bacteria, which are a normal part of the intestine, enter the vaginal mucosa and provoke inflammation.
Changes in the vaginal environment are also affected by:
- deficiency of female sex hormones - estrogens;
- diseases of the endocrine system;
- long-term use of antibiotics, OK (oral contraceptives) and antidepressants;
- decreased functioning of the immune system;
- uncontrolled relationships and frequent changes of sexual partners;
- congenital anomalies in the structure of the reproductive system;
- wearing synthetic underwear;
- inflammatory diseases in the renal structures and urinary system.
Symptoms of aerobic vaginitis
In the field of gynecology, several main stages in the development of vaginitis provoked by aerobic bacteria have been identified. The subacute form of aerobic vaginitis does not have a pronounced clinical picture. Therefore, treatment rarely begins in a timely manner. When the pathological process worsens, the following symptoms are observed:
- redness at the vaginal opening;
- the occurrence of copious discharge of a yellow tint that does not have a strong odor, in contrast to the bacterial type of pathology, characterized by a strong unpleasant odor;
- discomfort - itching and burning in the vulva area, intensifying at night;
- painful sensations during sexual intercourse.
Untimely treatment of the acute form of aerobic vaginitis provokes the transition of the disease into a chronic course. The pathology can last for several years without showing the characteristic symptoms of discomfort and pain.
But when the process worsens against the background of a sharp decrease in a woman’s immunity, pain and discomfort in the vaginal area make themselves felt.
Symptoms are especially pronounced in the period after the end of menstrual flow.
Diagnostics
Several types of laboratory tests help a gynecologist diagnose vaginitis caused by aerobic microflora in a woman. Bacterioscopic and bacteriological examinations are prescribed.
To carry out a bacterioscopic type of diagnosis, a smear of the vaginal microflora . It is sent to the laboratory, where special staining solutions and microscopic examination are carried out.
This technique is excellent for determining the types of aerobic microorganisms that cause the development of the inflammatory process. In addition to pathogens, an increased content of white blood cells is found in the vaginal microflora sample.
This is a basic sign of this type of vaginosis, since with bacterial vaginitis, the number of leukocytes remains normal.
Bacteriological examination is also carried out against the background of a selected smear of vaginal microflora. After taking a sample of biological material, it is placed in a nutrient medium for 24-48 hours.
Next, the crops are grown on nutrient media.
This type of study is less informative than bacterioscopic, due to the fact that those cultures of microorganisms that are part of the normal microflora of the vagina can also grow.
An integral part of the diagnosis, when diagnosing aerobic vaginosis, is a routine examination by a doctor on a gynecological chair using a special instrument - a speculum. Vaginitis, caused by aerobic bacterial microorganisms, leads to visible lesions of the mucous membranes lining the vagina.
It is important to note that women diagnosed with aerobic vaginosis do not always necessarily need treatment. Especially in cases where the microflora and the number of beneficial lactobacilli exceeds the percentage of pathogenic ones. Therefore, before starting therapy, the gynecologist must consult the woman about the further plan of action.
Treatment of aerobic vaginitis
Before developing a treatment regimen, the gynecologist must prescribe tests for sexually transmitted diseases. When making an accurate diagnosis, the treatment regimen is as follows:
It is important during diagnosis to identify the cause of inflammation. If the factor that triggered the development of aerobic vaginosis was endocrine disorders or hormonal imbalance, treatment will be based on eliminating these factors. Before starting treatment and during therapy, doctors strongly recommend abstaining from any sexual intercourse.
Just like with bacterial vaginitis, with aerobic vaginitis there is no need to treat the sexual partner, since this form of the disease does not affect men.
In addition to the above forms of treatment, to quickly restore the damaged integrity of the vaginal mucous membranes, sanitation or irrigation of the affected area with special solutions with an antiseptic effect is indicated.
chlorhexidine have good therapeutic activity against aerobic vaginitis . Medicines are produced in the form of tablets or vaginal suppositories. The main advantages of this type of drug are:
- reduced negative impact on the functioning of healthy parts of the mucous membrane;
- rapid disinfection of the vagina from all kinds of pathological secretions that occur with bacterial or aerobic vaginosis;
- influence on the removal of swelling at the site of the pathological process.
Depending on what form of aerobic vaginosis is diagnosed in a woman and how severe the pathology is, the duration of the course of therapy will differ. The chronic form of the disease takes much longer to treat than the acute form of the pathological process. For acute inflammation, the duration of therapy is from 7 to 14 days.
After completing the therapeutic course, gynecologists recommend douching . It is advisable to use preparations that contain lactic acid for vaginal irrigation. This will allow you to restore the damaged vaginal microflora as soon as possible. The douching course is individual. On average it is about 5 days.
Until the normal microflora of the vagina is fully restored, gynecologists recommend switching to a special diet. It is advisable to exclude spicy, smoked and sweet foods from the diet, and also avoid alcoholic beverages. After the course of treatment, the diet should be dominated by products of plant origin, as well as fermented milk products.
Self-medication for vaginitis of any etiology is not advisable. This is due to the fact that it is impossible to achieve the maximum therapeutic effect without accurately determining the factor provoking inflammation. In addition to the lack of effectiveness of traditional treatment methods, there is a risk of developing serious complications in the reproductive system.
Complications of aerobic vaginitis
The most serious complication of aerobic vaginosis not treated in a timely manner is the development of desquamative endocolpitis of inflammatory etiology. Aerobic vaginosis in women during pregnancy can cause the following complications:
- inflammation of the mucous membrane of the uterus and amniotic sac;
- premature rupture of membranes;
- constant miscarriages and inability to carry a child to term normally;
- earlier onset of the birth process.
If a woman, in addition to aerobic vaginosis, also has an infection in the urinary tract, in combination this can provoke the following complications:
- inflammatory processes in the fallopian tubes and uterine appendages;
- inflammation in the uterus of a chronic or acute course;
- development of adhesive processes in the pelvic organs.
Prevention
In order to prevent the development of aerobic vaginitis and prevent relapses after complete recovery, it is necessary to follow a number of recommendations and advice from gynecologists. Important rules for the prevention of vaginitis are:
- compliance with nutritional standards - food should be healthy, with the presence of a sufficient amount of lactic acid products;
- reducing your consumption of large amounts of sugar;
- wearing the right underwear made from natural fabrics;
- in case of casual sexual intercourse, be sure to use contraception;
- increase the body's immune strength;
- promptly treat infectious diseases of viral and bacterial etiology, especially if they affect the genital area.
By following these simple rules of prevention, a woman will be able to avoid serious complications caused by untreated aerobic type of vaginitis and maintain the health of her reproductive organs.
Source: https://tvojajbolit.ru/ginekologiya/aerobnyy_vaginit/
Pathogenesis of anaerobic infections
Anaerobic infections can usually be characterized as follows:
- They tend to appear as localized collections of pus (abscesses and cellulitis).
- Reduced O2 and low oxidation reduction potential, which predominate in avascular and necrotic tissues, are critical for their survival,
- When bacteremia occurs, it does not usually lead to disseminated intravascular coagulation (DIC).
Some anaerobic bacteria have obvious virulence factors. Virulence factors B.
fragilis are probably somewhat exaggerated due to their frequent detection in clinical specimens, despite their relative rarity in the normal flora.
This organism has a polysaccharide capsule, which apparently stimulates the formation of a purulent focus. An experimental model of intrabdominal sepsis showed that V.
fragilis can cause an abscess on its own, while other Bactericides spp. a synergistic effect of another organism is required.
Another virulence factor, a potent endotoxin, has been implicated in septic shock associated with severe Fusobacterium pharyngitis.
Morbidity and mortality in anaerobic and mixed bacterial sepsis are as high as in sepsis caused by a single aerobic microorganism.
READ MORE: Headache in right temple | Heart Health
Anaerobic infections are often complicated by deep tissue necrosis. The overall mortality rate in severe intraabdominal sepsis and mixed anaerobic pneumonia is high.
B. fragilis bacteremia has a high mortality rate, especially among the elderly and patients with cancer.
Diagnosis of anaerobic infection
For the timely diagnosis of anaerobic infection, the correct assessment of clinical symptoms is of great importance, allowing timely provision of the necessary medical care.
Depending on the location of the infectious focus, the diagnosis and treatment of anaerobic infection can be performed by clinicians of various specialties - general surgeons, traumatologists, neurosurgeons, gynecologists, otolaryngologists, maxillofacial and thoracic surgeons.
Methods for express diagnosis of anaerobic infection include bacterioscopy of wound discharge with Gram staining of a smear and gas-liquid chromatography.
In the verification of the pathogen, the leading role belongs to bacteriological culture of the discharged wound or abscess contents, analysis of pleural fluid, blood culture for aerobic and anaerobic bacteria, enzyme immunoassay, and PCR.
Biochemical blood parameters during anaerobic infection reveal a decrease in protein concentration, an increase in the level of creatinine, urea, bilirubin, transaminase and alkaline phosphatase activity.
READ MORE: What diseases are treated with oak bark