Absence of menstruation, scanty and infrequent menstruation: No. 91
In accordance with ICD 10, scanty periods can be observed with the following pathologies:
- Primary amenorrhea. It is observed in teenage girls due to constitutional characteristics or diseases of various organs. Experts include delayed sexual development, defects in the nervous system (central), abnormalities of the gonads and internal reproductive organs as the causes of primary amenorrhea.
- Secondary amenorrhea (hypogonadotropic, hypergonadotropic, normononadotropic). In this condition, women with a stable menstrual rhythm have no menstruation for 6 months or more. Secondary amenorrhea is caused by hypothalamic, adrenal, hypothalamic-pituitary, ovarian, psychogenic, and uterine factors.
- Amenorrhea, unspecified. The diagnosis is not associated with inflammatory processes. Menstruation is absent or scanty and infrequent.
- Primary oligomenorrhea. Menstrual irregularities according to the corresponding ICD code include short spontaneous periods with an interval of 36 days to 6 months. Signs of pathology are revealed during the formation of the menstrual rhythm.
- Secondary oligomenorrhea. Changes occur against the background of an established cycle due to various internal and external unfavorable factors.
- Oligomenorrhea, unspecified. Rare and scanty menstruation is a consequence of underdevelopment or depletion of the ovaries, immune disorders of unknown etiology.
Juvenile bleeding (uterine bleeding during puberty)
account for up to 10-37% of all gynecological diseases observed at the age of 12-18 years. In the pathogenesis of juvenile dysfunctional uterine bleeding, the leading role belongs to the infectious-toxic effect on the hypothalamic structures that have not reached functional maturity, which regulate ovarian function. Tonsillogenic infection has a particularly adverse effect. Mental trauma and inadequate stress on the nervous system, physical overload, malnutrition (both excessive and insufficient), and hypovitaminosis play a certain role.
Juvenile bleeding is characterized by a special type of anovulation, in which atresia of follicles that have not reached the ovulatory stage of maturity occurs. In this case, the synthesis of sex hormones in the ovaries is disrupted: estrogen production becomes relatively low and their level practically does not change throughout the menstrual cycle, progesterone is formed in small quantities. As a result, the endometrium does not undergo secretory transformation, which prevents its rejection and causes prolonged bleeding. At the same time, unlike hyperestrogenic menometrorrhagia, pronounced hyperplastic changes in the endometrium do not occur. Prolonged bleeding is also facilitated by insufficient contractile activity of the uterus, which has not yet reached final maturity.
Often girls are embarrassed to see a doctor for a long time, and thereby greatly harm themselves. Due to regular heavy blood loss, anemia occurs - a condition characterized by a decrease in the number of red blood cells (erythrocytes). They are responsible for the transport of oxygen to all organs and tissues; with their deficiency, a hypoxic state of the body develops. It is expressed by dizziness, weakness, decreased attention, and drowsiness. Moreover, if the problem of uterine bleeding is not resolved in a timely manner, the situation will only get worse.
Frequent, irregular, heavy periods: ICD 10 No. 92
Cycle disorders according to the ICD do not include bleeding that occurs after menopause. Heavy, irregular periods include:
- Frequent and heavy periods due to the regularity of the cycle. Gynecologists name menorrhagia and polymenorrhea as pathologies. With mennorrhagia, severe blood loss is observed in combination with an increase in the number of critical days. Within polymenorrhea, the cycle is less than 21 days.
- Frequent, heavy periods with irregular cycles. There are short intervals between critical days. The examination reveals menometrorrhagia (abnormal intense bleeding) and metrorrhagia.
- Copious bleeding during puberty. This item includes menorrhagia and bleeding that occurs during the puberty period.
- Bleeding of an ovulatory nature. There is regular blood loss, which often leads to anemia.
- Intense bleeding in the period before menopause. Gynecologists call metrorrhagia and menorrhagia that occur during the premenopausal, menopausal and menopausal stages.
- Other forms of irregular menstruation (specified).
- Irregular menstruation according to ICD 10 (unspecified). This section does not include pathological conditions with lengthening or shortening of the intervals between menstruation, scanty and heavy bleeding.
Heavy menstruation during puberty
ICD-10 code N92.2 for Heavy menstruation during puberty
Heavy bleeding at the beginning of the menstrual period Pubertal menorrhagia Pubertal bleeding
ICD-10
ICD-10-CM 10th Revision 2016
ICD-10-GM ICD-10 in Germany
ICD-10 ICD-10 in Russian
ICD-10
ICD-10 is the 10th revision of the International Statistical Classification of Diseases and Related Health Problems (ICD), a medical classification list by the World Health Organization (WHO).
It contains codes for diseases, signs and symptoms, abnormal findings, complaints, social circumstances, and external causes of injury or diseases.
The Anatomical Therapeutic Chemical (ATC) Classification System is used for the classification of active ingredients of drugs according to the organ or system on which they act and their therapeutic, pharmacological and chemical properties.
It is controlled by the World Health Organization Collaborating Center for Drug Statistics Methodology (WHOCC).
The defined daily dose (DDD) is a statistical measure of drug consumption, defined by the World Health Organization (WHO).
It is used to standardize the comparison of drug usage between different drugs or between different health care environments.
Painful periods: ICD 10 code No. 94
Painful periods according to ICD 10 mean:
- Pain that occurs approximately in the middle of the cycle.
- Dyspareunia. This disorder involves pain and discomfort during sexual intercourse. This item does not include psychogenic dyspareunia.
- Vaginismus. The disorder is understood as convulsive contractions of the vaginal muscles of a spastic nature that occur when attempting to examine or have sexual intercourse. Gynecologists do not include psychogenic vaginismus in this category.
- Syndrome of the so-called premenstrual tension. This is a complex of various symptoms characteristic of phase 2 of the cycle. PMS is individual in nature and usually includes psycho-emotional disorders and headaches.
- Primary dysmenorrhea. Painful menstruation is observed in women from menarche to the age of 30. The disorder is usually caused by hormonal disorders.
- Secondary dysmenorrhea. Pain that accompanies menstruation often appears due to gynecological diseases.
- Dysmenorrhea (unspecified). This diagnosis can be made for menstrual pain of unknown etiology.
- Other conditions (specified) that are directly related to the menstrual cycle and reproductive organs.
- Unspecified pathologies associated with the cycle and genitals.
Causes of menstrual cycle disruption: what do irregular “these days” mean?
Menstruation is an indicator of the rhythm of hormone release. Sometimes a woman may not be aware of the existing pathology, but an experienced doctor will regard menstrual irregularities as a symptom. An increase or decrease in blood volume, a change in the duration of bleeding, and the time intervals between them are possible. As a rule, the causes are functional in nature or associated with organic changes.
Treatment of pathology of menstruation should be carried out by an obstetrician-gynecologist. But sometimes the cause of the failure is changes in the endocrine system and the brain. Then endocrinologists, therapists, neurologists, neurosurgeons and even psychotherapists are involved in therapy.
What is considered normal
To determine the signs of a menstrual cycle disorder, you need to understand what is included in the concept of normal. For each woman, this is individual, but there are boundaries, if violated, you need to look for pathology.
- Cycle duration. The average is 28 days. Doctors rely on it when calculating the phases of the cycle, the day of ovulation, and menstruation. But cycles from 21 to 35 days also fit into the normal parameter.
- Period . Menstrual bleeding accounts for an average of four to five days of the total duration of the cycle. But it can also be three to seven days of menstruation. The main condition is the same duration every month.
- Amount of bleeding. Blood loss should not exhaust the body. Bleeding not exceeding 100 ml is considered physiological. There are special tables or graphic diagrams by which you can calculate your blood loss, focusing on the appearance of the pads and their number per day.
- Ovulation. Normally occurs in the middle of the cycle. Only in young girls with an unsteady cycle and in women before menopause, most of the menstruation occurs without ovulation. Healthy women can also have cycles without egg maturation, but much less frequently.
- Discharge. Physiological leucorrhoea is no more than 20 ml per day of whitish mucus. Before ovulation, its amount increases. The appearance of bloody discharge, an unpleasant odor, and an increase in volume should alert you.
Heavy menstruation and bleeding during puberty
Patients of any age can experience heavy bleeding from the uterus. Normally, the volume of blood that is lost during menstruation does not exceed 60-80 ml. If the blood loss is greater, we are no longer talking about menstruation, but about hypermenorrhea - pathologically heavy menstruation or menorrhagia, that is, regular bleeding that occurs on the days of menstruation. The difference between them is the number of days: heavy menstruation fits into the normal duration of menstruation - 7-10 days, while uterine bleeding lasts longer, up to 10-14 days.
The causes of uterine bleeding are divided into two large groups:
Menstrual irregularities: types
Disorders of the ovarian-menstrual cycle can be either in the direction of its decrease or increase. And sometimes bleeding ceases to follow any rhythm at all and comes at a new time each time. In the international classification ICD-10, menstrual cycle disorders fit into category N92. It covers frequent, heavy, irregular menstruation. This also includes bleeding during puberty (N92.2), during ovulation (N92.3) and before menopause (N92.4).
Hypermenstrual syndrome
Each type of violation has its own name. In case of hypermenstrual syndrome, when there is an increase in the duration or volume of blood loss, the following types of pathological menstruation are distinguished:
- polymenorrhea - prolonged bleeding during menstruation, which passes into the uterus;
- hypermenorrhea - a large amount of blood loss during menstruation;
- proyomenorrhea - frequent, long and heavy periods.
Hypomenstrual syndrome
Changes to a lesser extent are combined into hypomenstrual syndrome. It includes the following concepts:
- oligomenorrhea - short menstrual bleeding for one to two days;
- hypomenorrhea - scanty discharge during menstruation;
- opsomenorea - 40-50 days pass between bleedings;
- amenorrhea - no periods for six months or more.
Reasons for changes
The reasons for the disruption of the menstrual cycle can be both external and internal. Female hormonal levels depend on the general level of health and emotional state, because there is a subtle connection with the cortical structures of the brain. The levels of serotonin and melatonin, the concentration of adrenaline can affect sex hormones and lead to changes in the cycle. But with each failure, the mechanism of development of the pathology will be different, which will require different approaches to treatment.
Infection
Acute or chronic infectious diseases of the pelvic organs can lead to serious consequences. Menstrual bleeding may be more intense and the intervals between them irregular. With chlamydia and chronic gonorrhea, the condition of the endometrium changes; it becomes more loose and swollen. Therefore, the separation of the endometrium during menstruation is delayed for a longer period, pain appears, and bleeding becomes profuse. With chronic infections of the genital tract, delays in menstruation and dyscirculatory uterine bleeding may occur.
Endometriosis
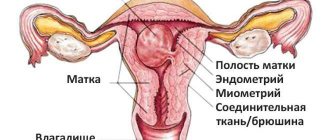
Endometrial lesions have their own hormonal activity, but they are subject to the same cyclical changes as normal tissue. If endometriosis affects the body of the uterus, the lesions grow deep into the muscles and form cavities that resemble honeycombs. They take longer to empty than the uterus itself, so menstruation lasts a long time, the blood at the end becomes dark.
With endometriosis, there is an increase in the number of pain receptors around the lesions. Menstruation and the intervals between them are accompanied by pain. An increased amount of estrogen leads to endometrial hyperplasia, so there may also be bleeding between menstruation.
Myoma
Failure of the menstrual cycle with small uterine fibroids is associated with an imbalance of hormones. If the neoplasm has grown to a large size and deforms the uterine cavity, then the contractility of the myometrium is impaired, and the mucous membrane is separated worse. Nodes located interstitially or submucosally increase the area of the inner surface of the uterus. The endometrium grows much larger; its separation will take not five to seven days, but 10-12.
Polycystic ovary syndrome
Polycystic ovary syndrome is a hormonal disease in which the final maturation of the follicle does not occur. They remain on the surface of the ovary in the form of small cysts. The absence of ovulation does not lead to an increase in progesterone; the endometrium does not undergo the necessary transformations. Therefore, menstruation appears rarely, with long delays.
Climax
Disruption of the menstrual cycle during menopause occurs due to the gradual inhibition of ovarian function. The synthesis of estrogen decreases, so the intervals between menstruation increase and delays occur. Gradually, periods come once every few months and at one point stop completely. If spotting does not appear throughout the year, then the date of the last menstruation is taken as the moment of menopause.
Abortion and childbirth
Termination of pregnancy, regardless of the method and duration, is severe stress for the body. The longer the period in which the abortion was performed or the miscarriage occurred, the higher the likelihood of failure. Pregnancy is a complex process of restructuring the entire body. If a woman has an abortion, then the hormonal system loses its guidelines. In a short term, removal of the fertilized egg and trophoblast leads to a sharp decrease in progesterone. This requires a response from the pituitary gland - stimulating the production of estrogen in order to restore the endometrium and begin to grow a new follicle. Sometimes this process is delayed and the cycle gets disrupted.
Causes of the pathological phenomenon
What causes the appearance of hyperpolymenorrhea depends in some cases on its type. Infections and stress have a strong impact on the body of adolescents, making primary pathology more possible. The same can happen with hereditary problems with blood clotting and genetically determined characteristics of menstruation, when the girl’s mother and grandmother had the same problem. But in general, menorrhagia has broader causes:
- Periods of hormonal changes. We are talking, of course, about teenagers, but also about women who have recently experienced childbirth, as well as those who are on the verge of menopause. In the latter case, the ICD encrypts the pathology under code No. 92.4.
- Use of intrauterine contraception. Spirals and candles may have side effects.
- Endocrine pathologies, liver and kidney diseases, cardiac problems. All affect hormonal status.
- Pathologies of the reproductive system. This cause of the syndrome combines polyps, adenomyosis, and ovarian diseases. If uterine fibroids are diagnosed, menorrhagia can also be combined with metrorrhagia.
- Hard physical work, frequent changes in climatic conditions. All this is a serious test for the body.
- Incorrect use of medications or period of adaptation to them. These may be hormones and blood thinners.
https://youtu.be/unWtItWztNQ
How can you influence the cycle?
Treatment of menstrual irregularities depends on the causes of the disease. Therefore, high-quality diagnostics are necessary, which includes:
- medical examination;
- hormone tests;
- Ultrasound of the pelvis.
Additional methods depend on the data obtained at the initial stage. The treatment uses an integrated approach.
- Pills . Medicines prescribed for menstrual irregularities most often belong to the group of hormones. In case of luteal phase deficiency, Duphaston, Utrozhestan or progesterone injections are used. For hyperprolactinemia, Bromocriptine and Dostinex are used. If Sheehan syndrome has developed, then complex hormonal treatment is necessary.
- Vitamins. Vitamin therapy for menstrual irregularities involves prescribing a complex of active substances or individual vitamins A, E, C, as well as folic acid. Some doctors suggest distributing them depending on the hormonal phase.
- Folk remedies. Herbal treatment can be used to normalize the cycle. The hog uterus can increase the volume and duration of bleeding. And nettle, on the contrary, is reduced. Chamomile is used as an anti-inflammatory agent. But with serious hormonal imbalances, herbal remedies are powerless.
- Hirudotherapy. According to reviews, leeches can be effective for endometriosis. But you shouldn’t place high hopes on this technique. It can only complement the main treatment. Like homeopathy, hirudotherapy has a placebo effect, so there is debate about its effectiveness.
To avoid signs of menstrual irregularities, it is necessary to take care of prevention. It includes protection from sexually transmitted infections, protection from unwanted pregnancies instead of subsequent abortions. Proper nutrition, emotional balance and treatment of concomitant diseases will preserve reproductive health.
Diagnosis of pathology
The occurrence of menorrhagia-type NMC should convince the woman to go to a specialist. He will find out the circumstances after which the syndrome was discovered and examine the patient in the chair. If this is not enough, the following are indicated to determine the cause:
- Ultrasound of the pelvis;
- hysteroscopy;
- curettage and examination of the organ mucosa;
- laboratory blood tests for biochemistry and hormones, coagulogram, identification of tumor markers CA 19-9, CA-125;
- cytological examination of cervical tissue.
Reviews
I started having this problem about 1 year ago. The cycle has completely broken down. My period doesn't come for 4 months. When I started visiting doctors, I was told that there were problems either with hormones or with the ovaries.
Alyona Sinica, https://detkam.su/forum/57-606-1
I think it's hormonal. I had this after I got nervous when I was studying at the university, the delay was 2 weeks, I already ran to the gynecologist, I thought I was pregnant, but everything turned out okay. Irregular periods can be due to depression, nervousness and other feminine troubles.
My menstrual cycle was restored when I started eating foods containing iodine (seaweed, etc.). I have been a vegetarian for more than four years.
Clinics for treatment with the best prices
Price
Total: 394in 26 cities
| Selected clinics | Phones | City (metro) | Rating | Price of services |
| MEDSI on Leningradsky Prospekt | +7(495) 229..show+7(495) 229-18-75+7(495) 152-55-46 | Moscow (m. Airport) | — | 25930ք (80%*) |
| MEDSI on Leninskaya Sloboda | +7(495) 023..show+7(495) 023-60-84 | Moscow (m. Avtozavodskaya) | — | 25930ք (80%*) |
| MEDSI in Khoroshevsky Proezd | +7(495) 780..show+7(495) 780-40-64+7(495) 152-55-46 | Moscow (metro station Begovaya) | — | 25930ք (80%*) |
| MEDSI in Butovo | +7(495) 023..show+7(495) 023-60-84 | Moscow (metro Dmitry Donskoy Boulevard) | — | 25930ք (80%*) |
| MEDSI on Rublevskoe highway | +7(495) 023..show+7(495) 023-60-84 | Moscow (metro station Kuntsevskaya) | — | 25930ք (80%*) |
| MEDSI on Prechistenka | +7(495) 739..show+7(495) 739-53-67+7(495) 152-55-46 | Moscow (metro Park Kultury) | — | 25930ք (80%*) |
| MEDSI on Dubininskaya | +7(495) 737..show+7(495) 737-01-90+7(495) 152-55-46 | Moscow (metro Paveletskaya) | — | 25930ք (80%*) |
| MEDSI in Krasnogorsk | +7(495) 730..show+7(495) 730-57-15+7(495) 152-55-46 | Krasnogorsk (metro station Pyatnitskoe highway) | — | 25930ք (80%*) |
| MEDSI on Leninsky Prospekt | +7(495) 023..show+7(495) 023-60-84 | Moscow (metro station Shabolovskaya) | — | 25930ք (80%*) |
| MEDSI in Mitino | +7(495) 023..show+7(495) 023-60-84 | Moscow (metro station Pyatnitskoe highway) | — | 26060ք (80%*) |
| * – the clinic does not provide 100% of the selected services. More details by clicking on the price. | ||||
Source
Algomenorrhea: what is it in women
Quite a large number of women around the world suffer from painful sensations during menstruation. Some of the fair sex experience this sensation from the moment of menarche, that is, the first day of their first menstruation in their lives.
In some cases, painful sensations during menstruation can be harbingers of some truly serious pathological conditions, and many of them can seriously harm health without timely medical intervention.
What is algomenorrhea?
The pathology of algodismenorrhea is a disorder of the ovarian-menstrual cycle, which is characterized by the presence of painful menstruation. Algodysmenorrhea is not a diagnosis, but only a condition that appears for various reasons.
Algomenorrhea and its types
Indeed, there are many women who feel this condition since the start of menstruation. If these symptoms are not associated with organic lesions, then the nature of such algodismenorrhea is functional, and this is what is called primary algodismenorrhea. Primary algomenorrhea is caused by increased production of prostaglandins in the woman’s body. In this case, a non-steroidal anti-inflammatory drug can be used a few days before the day of the expected menstruation. This group of drugs block the release of prostaglandins, and accordingly prevent such strong and painful uterine contractions. Contraceptives can be used for algomenorrhea to correct hormonal levels.
Types of menorrhagia and their manifestations
Menstruation that lasts over a week and forces you to change hygiene products every hour or two or more often occurs in 30% of women. This is a mixed age group. In accordance with this, the syndrome is divided into types. Although menorrhagia ICD is united under the general code No. 92.0.
Primary
Menstruation sometimes from adolescence is characterized by a large amount of discharge and duration. For some, this occurs with menarche, while others discover the syndrome when menstruation occurs for the second and subsequent times. Such menorrhagia (ICD code 92.2) is designated as “Heavy menstruation during puberty.”
Young age is characterized by hormonal instability. The amount of estrogen can significantly exceed the norm throughout the cycle, and gestagens are in short supply. This is the reason for the diagnosis of “primary menorrhagia”. An excess of some and a deficiency of other substances lead to the preservation of endometrial thickness in the second phase of the cycle. When it begins to be rejected, there are many tissues to be replaced, just like capillaries and blood. The development of the mucous membrane is uneven, so its detachment takes a long time. If there is underdevelopment of the uterus, its low ability to contract also contributes to menorrhagia.
Secondary
Not only teenagers suffer from heavy and long periods. And in adult girls and women, after many normal cycles, idiopathic menorrhagia may occur. It is caused by the appearance of developmental disorders of the uterine mucosa caused by various reasons. This type of painful syndrome is secondary.
How to distinguish simply heavy periods from a pathological condition? Menorrhagia symptoms are clear and easy to identify:
- the process lasts more than a week;
- the discharge is characterized by a large volume, the presence of clots, and remains like this throughout the entire period of menstruation, at night;
- the amount of blood lost exceeds 150 ml, and the amount of pads used per day is more than 10 pieces;
- severe weakness is felt, which goes away a little after the bleeding stops;
- the cycle is shortened in time.
The discharge detected during the syndrome is precisely menstrual, that is, it occurs on schedule and after the disintegration of the unfertilized egg. Do not confuse the concepts of menorrhagia and metrorrhagia. The latter means intense secretions not associated with the maturation of the germ cell. However, both syndromes often coexist.
Algomenorrhea: code according to ICD 10
There is an international classification that includes a list of all pathological conditions, which are divided into categories and assigned their own codes. Doctors all over the world, through this classification, can immediately determine what type of disease a woman has using the specified code.
This condition has its place in the International Classification of Diseases, 10th revision.
This pathological condition belongs to a heading called N. Subsection 94.
The number N94.0 encodes pain that occurs in the middle of the menstrual cycle.
This pathological condition is hidden under the code N94.1. Like dyspareunia, that is, painful sexual intercourse due to a large number of nuances. Which can give symptoms of varying severity. However, this section does not include such a nosology as dyspareunia of a psychogenic nature. All such conditions associated with mental disorders are encoded in heading F. Namely F52.6, denoting psychogenic dyspareunia. This is an exclusively psychiatric field that obstetrician-gynecologists cannot fight.
N94.2 in this group, this code hides a pathological condition such as vaginismus. This is a contraction of the muscles of the vestibule of the vagina, which interferes with normal sexual relations. Corresponding to the previous state. Psychogenic vaginismus belongs to a completely different subgroup and is coded as F52.5. This condition requires an integrated approach both from gynecologists, but more from neurologists and psychiatrists.
Algodismenorrhea: microbial 10
Primary algomenorrhea ICD code 10 has heading N 94.4. a condition characterized by painful menstruation from adolescence. The pain can also have varying intensity, but is present almost from the moment the girl’s first menstruation in her life.
Secondary algodismenorrhea, ICD 10 code has N94.5 and is characterized by acquired nuances of pain during menstrual bleeding.
This means that for some time the woman did not complain about such symptoms during the endometrial desquamation phase, but at a certain moment she felt pain of varying intensity.
Unspecified algomenorrhea is defined by ICD 10 as N94.6.
In addition to the division approved by the International Classification of Diseases, Tenth Revision, there is also a distribution of such conditions according to the severity of the condition.
- Compensated algodismenorrhea, which does not change its signs of pain severity over time.
- The decompensated form of this condition is characterized by an increase in the intensity of symptoms, leading to a disruption in the quality of life of the fair sex.
Attention!
- By self-medicating, you can cause irreparable harm to your health.
- The information posted on the MedElement website and in the mobile applications “MedElement”, “Lekar Pro”, “Dariger Pro”, “Diseases: Therapist’s Guide” cannot and should not replace a face-to-face consultation with a doctor. Be sure to contact a medical facility if you have any illnesses or symptoms that concern you.
- The choice of medications and their dosage must be discussed with a specialist. Only a doctor can prescribe the right medicine and its dosage, taking into account the disease and condition of the patient’s body.
- The MedElement website and mobile applications “MedElement”, “Lekar Pro”, “Dariger Pro”, “Diseases: Therapist’s Directory” are exclusively information and reference resources. The information posted on this site should not be used to unauthorizedly change doctor's orders.
- The editors of MedElement are not responsible for any personal injury or property damage resulting from the use of this site.
Bleeding from the genital tract is considered normal, which appears at intervals of 21-35 days and lasts from three to six days. If the regularity or volume changes, then there must be a pathological reason for the cycle failure. Metrorrhagia is the occurrence of bleeding from the genital tract outside of normal menstruation. This symptom can appear at any age - in adolescents, women of reproductive age, during menopause.
The ICD-10 code for metrorrhagia corresponds to several categories. N92 includes heavy, irregular and frequent menstruation, and N93 includes other abnormal bleeding from the uterus that may occur after coitus (N93.0) or for unspecified reasons (N93.8-9).
Algomenorrhea: treatment, drugs
Before treating painful menstruation, a woman must consult an obstetrician-gynecologist for a comprehensive examination and identify the cause. Why the process of menstruation is painful. If, based on the results of the examination, the cause, as such, was not identified, then we can talk about true algodismenorrhea and fight against it. The cause of too painful menstruation is increased synthesis and release of prostaglandins.
It is in order to block this source of discomfort that nonsteroidal anti-inflammatory drugs (ibuprofen, nurofen, amelotex) are prescribed. And also antispasmodics in the form of platyphylline, drotaverine (no-shpy), spasmalgon.
Treatment of juvenile uterine bleeding.
To stop moderate bleeding, hormonal contraception is used. For this purpose, estrogen-gestagen drugs (monophasic combined oral contraceptives) or pure gestagens are used according to the scheme until bleeding stops. In addition, it is advisable to use drugs that increase blood clotting, as well as non-steroidal anti-inflammatory drugs. In addition, all patients with juvenile bleeding are required to be prescribed antianemic therapy with iron supplements.
Surgical treatment (curettage of the mucous membrane of the uterine cavity) is used extremely rarely in young patients, only if the bleeding threatens the girl’s life and cannot be treated conservatively.
In addition to treating bleeding that has already occurred, it is advisable to prevent the recurrence of juvenile dysfunctional uterine bleeding. It is aimed at the formation of a regular ovulatory menstrual cycle, is carried out with estrogen-progestin drugs (COCs), and is prescribed for at least three months to stabilize the menstrual cycle.
Any treatment for such conditions should be carried out by a gynecologist. in addition, girls who have been successfully treated for uterine bleeding during puberty should be under the supervision of their attending physician until the end of puberty.
Prevention of algomenorrhea
In order to eliminate painful menstruation, it is necessary to prevent gynecological pathologies that lead to such consequences, as well as regularly visit an obstetrician-gynecologist to identify processes in the early stages. In case of true algodismenorrhea, it is indicated 2-3 days before the date of expected menstruation to start taking non-steroidal anti-inflammatory drugs as blockers of the adverse effects of prostaglandins on the reproductive and, very importantly, the nervous system.
Information
Sources and literature
- Protocols for the diagnosis and treatment of diseases of the Ministry of Health of the Republic of Kazakhstan (Order No. 764 of December 28, 2007) List of used literature: 1. The J. Hopkins Manual of Gynecology and Obstetrics // Ed. By N. Lambrou, A. Morse, E. Wallach, 1999. 2. PRODIGY Guidance – Menorrhagia Last revised in July 2005 3. Am Fam Physician. 2005 Jan 15;71(2):285-91. Dysmenorrhea. French L. Department of Family Practice, Michigan State University, College of Human Medicine.
Information
List of developers:
Sultanova Zh.U. Candidate of Medical Sciences, Senior Researcher Republican Research Center for Maternal and Child Health (RNICMHMR)