Norm or pathology
The body of a healthy woman of reproductive age undergoes cyclical changes every month associated with changes in hormonal regulation at the level of the pituitary gland and ovaries. And during certain periods, discharge is observed in the intimate area of women. As a rule, this discharge is not accompanied by any additional symptoms, but sometimes women experience additional symptoms in an intimate place, for example, burning or itching with vaginal discharge. In each specific case, it is necessary to understand what causes such symptoms.
Gynecological diseases
Women's discharge varies. It is believed that in the absence of pathology, a transparent vaginal secretion should be observed, while it does not smell or cause discomfort. Any deviations from the norm are already a sign of the development of an infectious process that requires immediate treatment.
There are many microorganisms present in the vagina, which are divided into “good” and “bad”. There is a balance between them, which can be disrupted when exposed to certain factors, which is why “bad” microorganisms begin to actively multiply, provoking the development of diseases.
Among them is candidiasis. This disease is caused by fungi of the genus Candida and is manifested by copious white vaginal discharge with the smell of sour milk. In this case, the skin becomes irritated, itching appears, which is complemented by a burning sensation when urinating, the genitals become red and swollen. The copious discharge itself can be different - thick, liquid, homogeneous, or contain lumps.
But most often they resemble a curd mass or are presented in the form of white flakes. In this case, a woman may experience other symptoms, for example, a burning sensation when urinating, flaking of the skin in the perineal area, the appearance of a white coating on the labia, etc.
Due to the fact that the discharge provokes constant discomfort in the intimate area, the woman becomes irritable, has mood swings, and complexes appear.
During thrush, it is strictly forbidden to have sex with a man, since this disease can be transmitted from one partner to another and then both will have to be treated.
Allergic reactions
Under normal cycle conditions, female discharge varies quite a lot in consistency, viscosity, thickness, color and shade. This must be taken into account when deciding whether these discharges are normal or whether you still need to contact a specialist. Yellow discharge in women is not always considered pathological. Sometimes yellow discharge and itching can be caused by a banal vaginal allergy to intimate hygiene products, vaginal contraceptives, tampons, or male sperm. It may also be a local allergic reaction to medications taken orally. As a rule, a yellowish, odorless discharge appears. Before declaring war on such symptoms, you should first change all hygiene products and other factors that come into contact with the female intimate area.
Improper hygiene
Sometimes in women, discharge and itching in the intimate area can be caused by a simple violation of personal hygiene rules. Sometimes the presence of foreign elements (remnants of tampons, pads) can provoke an inflammatory reaction. Infrequent hygiene measures contribute to the occurrence of excessive growth of microflora on the mucous membranes of the external genital tract and vagina. If, after excluding all allergic and hygienic factors, a woman’s itching and discharge persist, then she should visit a gynecologist to take smears from three points and conduct a bacterial culture.
STD
Sexually transmitted diseases have a pronounced symptomatic picture. However, it does not appear immediately. Often, at the very beginning of its development, an STD is asymptomatic, but as soon as the immune system weakens or some chronic disease worsens, signs of a sexually transmitted infection appear right there. Moreover, quite often they manifest themselves with symptoms such as:
- itching, burning, tingling in the intimate area;
- redness of the skin, peeling;
- swelling;
- painful pulling sensations in the lower abdomen;
- pain when urinating, etc.
Bacterial vaginosis
Currently, bacterial vaginosis is the most common cause of pathological, odorless discharge with itching in women of childbearing age. This pathology can have a significant impact on quality of life and psychological well-being if it is repeated and is characterized by severe symptoms such as itching in intimate places in women with discharge and a fishy odor.
Often with vaginosis, gardnerella is present in smears. The opinion of the medical community about Gardnerella is very controversial. On the one hand, this pathogen is considered the causative agent of bacterial vaginosis, on the other hand, there is an opinion that gardnerella itself is not dangerous, but exhibits its pathological effect only in combination with other opportunistic microorganisms. Several studies over the past decade support the concept of bacterial vaginosis as a sexually transmitted infection.
The course of bacterial vaginosis varies greatly among women. Some have asymptomatic bacterial vaginosis, others experience odorless itching, and others experience a fishy odor, which may intensify during menstruation. Bacterial vaginosis usually responds to antibiotic treatment, but can recur quickly, with some reports suggesting recurrence rates of more than 50% within 3-6 months.
Some studies suggest that vaginosis factors are sexually transmitted, and in this case, more pathogenic strains of Gardnerella are identified. Bacterial vaginosis is a risk factor for adverse pregnancy outcomes, including second trimester miscarriage, spontaneous preterm birth, and cesarean section.
There is a concept that describes the vaginal microbiota as a single organism - a biofilm. Many researchers have noted the great genetic diversity of different strains of Gardnerella, including the presence of their non-pathological varieties. Differences have been described in several genes and virulence factors, such as adhesion, cytotoxicity, and biofilm formation ability. There are attempts to divide all Gardnerella into 4 different species.
There is a version of the medical community about the increase in the level of resistance of bacterial vaginosis agents to metronidazole, and the emergence of metronidazole-refractory bacterial vaginosis. A 2014 study compared the ability of Gardnerella and 30 other BV-associated bacteria to form biofilm, adhere to epithelial cells, and induce cytotoxicity. Gardnerella was the most pathogenic, confirming its central role in pathogenesis.
The presence of pockets of biofilm persisting after antibiotic treatment and subsequent recovery has led Western researchers to explore a method of biofilm removal to achieve complete cure for bacterial vaginosis. Relapse was caused by persistence of pathological biofilm, recolonization from the intestine or through a partner. Prebiotics are effective in restoring lactobacilli, but long-term treatment may be required to maintain healthy vaginal flora.
Important! A new treatment regimen for vaginosis in Western countries includes dequalinium chloride (an antiseptic), which also has activity against Candida fungus and is useful for women who often suffer from vaginosis and candidiasis.
A recent study in Belfast found that rectal specimens detected Gardnerella in 83.2% and Mycoplasma hominis in 24.3% of all cases. This means that the source of microbial colonization of the vagina could theoretically be the contents of the intestines. It has also been shown that gardnerella is capable of colonizing the male urethral canal with the formation of biofilms.
Candidiasis
If discharge and itching are observed in a woman with a weakened immune system, and at the same time there is a cheesy discharge with an unpleasant, sour odor, then the woman is most likely suffering from vaginal candidiasis. This is a very unpleasant disease, a common symptom of which is severe itching in the perineum, vagina and external genitalia. Itching is often observed before menstruation, the woman constantly itches, becomes nervous, irritable, and suffers from insomnia. However, the treatment of such a disease is quite effective.
The prescription of antifungal drugs and restoratives, the elimination of risk factors and causes leading to a decrease in immunity, causes regression of such unpleasant symptoms. The exception is for persons with persistently weakened immunity, especially with HIV infection. In this case, treatment is long and difficult: it requires the prescription of antiretroviral drugs and immunomodulators. Such patients should be regularly examined and repeated courses of therapy.
Cervical erosion
Cervical erosion is an ectopia of columnar epithelium beyond the cervical canal to the outside. The main function of the columnar epithelium of the cervical canal is the secretion of mucus, which moisturizes the vagina, and during pregnancy, the creation of a mucus plug that isolates the uterine cavity from the external environment and prevents infection of the fetus.
Important! Some researchers in the West consider such a disease to be a variant of the norm that does not require unnecessary actions.
Previously, it was believed that erosion was the result of poor hygiene or infection. Now the endocrine theory prevails, according to which hormonal changes in the body of a nulliparous woman can provoke ectopia. For those who have given birth, the cause of erosion can be childbirth and micro-tears. Exacerbating factors are believed to be:
- sexual infections;
- frequent change of partners;
- congestion in the pelvis.
Symptoms of erosion may include pain in the lower abdomen, odorless discharge in women with itching, and a rash on the external genitalia. But usually these are not direct signs of erosion, but the result of associated infection and/or inflammation. Diagnosis is carried out by colposcopy. Modern treatment includes douching, medicinal applications, and treatment of associated infections.
Inflammation of the genital organs
In the lives of most women, inflammatory diseases of the reproductive system are present. The most common of them are:
- adnexitis;
- salpingo-oophoritis;
- oophoritis;
- colpitis;
- vaginitis and others.
Most often, they are caused by opportunistic flora, and provoking factors include hypothermia, frequent changes of sexual partners, decreased immunity, neglect of personal hygiene rules and other factors. The clinical picture is pain in the lower abdomen, clear discharge, or profuse mucous leucorrhoea. Sometimes the discharge may be yellow and odorless. The diagnosis is made based on examination of a vaginal smear, bacteriological culture, and pelvic ultrasound data.
Endometriosis
Endometriosis is the growth of the endometrium beyond the physiologically designated area. With this disease, the endometrium can not only expand deep into the thickness of the uterus, but also extend beyond its limits, often found in the pelvic cavity: on the peritoneum, rectum, ovaries, fallopian tubes, and bladder.
Endometriosis is a hormonal-dependent disease. Its tissues undergo the same cyclic changes as the normally located endometrium. Brown discharge in women outside of menstruation, pelvic pain, anemia, and infertility are often observed. One of the complications of this disease is bleeding. Clinical manifestations largely depend on the location of endometrial ectopia. After inflammatory processes and uterine fibroids, endometriosis is the most common gynecological problem.
The cause of endometriosis is considered to be retrograde menstruation, or the implantation of separated endometrium outside the uterine cavity. Pregnancies, abortions, cesarean sections, surgical interventions, and exercises associated with increased pressure in the abdominal cavity provoke this disease. Diagnosis of endometriosis may include: gynecological examination, colposcopy, hysterosalpingoscopy, ultrasound, laparoscopy, hysterosalpingography. Treatment options include surgery and hormonal therapy.
Venereal diseases
Sexually transmitted diseases often have mild symptoms, and the itching may be mild. Chlamydia and ureaplasma usually develop without discharge, and the only symptoms may be a burning sensation in the vagina and mild itching. Severe itching with watery, painful blisters is most likely caused by genital herpes.
Gonorrhea often occurs latently in women, and trichomoniasis causes profuse brownish discharge. Therapy for such diseases is prescribed by a venereologist; the treatment regimen is selected taking into account the nature of the pathogen and its sensitivity to certain medications.
Yellow curdish discharge without odor
Yellow discharge, like cottage cheese, often appears during inflammatory processes of the internal genital organs, namely with infectious pathologies of the ovaries, fallopian tubes, and the like. In the case of acute inflammation, a woman notices the appearance of copious vaginal secretions without the characteristic unpleasant odor that occurs when bacterial pathogenic flora is attached and pus appears.
Among the symptoms of inflammatory processes in the area of the appendages, ovaries, and fallopian tubes are:
- pain in the lower abdomen and perineum;
- increase in general body temperature;
- the appearance of discomfort during urination and sexual intercourse;
- itching and burning in the vagina;
- menstrual irregularities;
- uterine bleeding;
- anovulatory menstrual cycle (lack of ovulation) and infertility.
Other reasons
The causes of pathological vaginal discharge can be very different. Thus, brown discharge and itching can be observed with cervical polyps. During sexual intercourse, polyps may be traumatized and mild bleeding may occur from them.
Important! Another reason may be endocrine disorders, leading to dysregulation of the cycle and the occurrence of atypical discharge.
Hormonal contraceptives can also change normal leucorrhoea. Thus, oral contraceptives suppress ovulation, as a result of which the usually observed profuse, lasting discharge during ovulation becomes more scanty and loses its characteristic consistency.
In the course of her life, every woman must have the skills of self-observation so as not to miss a possible pathology. If atypical discharge appears, she should make a decision on further actions together with her doctor. In no case should you self-medicate, since only a specialist will be able to determine the nature of therapy, its volume and prevent complications.
White or whitish-transparent discharge without a strong odor in women is normal and does not require treatment. Things are different when there is itching in the intimate area, white, brown, yellow, greenish and purulent discharge with an unpleasant odor. Their appearance indicates the development of a pathological process in the body, which certainly requires treatment. Leucorrhoea and itching in women are a very common problem that requires timely treatment.
Main reasons
Various factors can provoke discomfort in the perineum and excessive production of vaginal secretions. They are conventionally divided into 2 groups:
- Infectious.
- Physiological.
In the first case, the role of provocateurs is various viral agents, the active activity of which leads to changes in the microflora of the vagina. In the second, we are talking about the impact of negative internal or external factors that have no connection with infectious processes. However, this does not mean that the discharge and itching that appears against it do not require treatment. Sometimes, such symptoms indicate serious disturbances in the functioning of the body, which can disable its functioning.
Infectious
When pathogenic flora begins to predominate in the vagina, a change occurs in the composition of the mucous secretion produced by the cervix. It acquires a specific smell and a different shade. The body tries to cope with the infection on its own, trying to “wash” it out of the vagina, which is manifested by an increase in the synthesis of exudate. It, in turn, irritates the mucous membranes and skin of the external genitalia, which manifests itself in the form of itching.
The following may act as infectious agents:
- Fungi of the genus Candida.
- Chlamydia.
- Gonococci.
- Herpes.
- Trichomonas.
- Mycoplasma.
- Ureaplasma, etc.
All of these STD pathogens are characterized by copious discharge and itching of the labia. However, the general symptoms differ. So, for example, with a fungal infection the following picture is observed:
- Unbearable itching and burning in the perineum.
- Swelling and redness of the labia.
- Increased production of white discharge (it can be either curd-like consistency or liquid).
- The smell of sour milk.
When chlamydia is the cause of such a clinical picture, the main symptoms are supplemented by:
- Changes in the color of vaginal secretions (it becomes dark gray or yellow).
- Increased concentration of secretions.
- The appearance of a pungent odor.
- Swelling and peeling of the genitals.
Gonococci provoke the development of a disease such as gonorrhea, which manifests itself in the form of:
- Severe itching and burning in the vagina.
- Yellow discharge that depletes the fishy aroma.
- Painful sensations in the lower abdomen, aggravated by sexual intercourse.
- Pain while urinating.
Genital herpes provokes not only the appearance of itching and increased vaginal discharge, but also the appearance of small rashes on the genitals, which resemble small blisters filled with liquid. In this case, as a rule, there is no specific aroma. The rash disappears after 10-14 days, but this does not indicate complete recovery. You will need to take a course of antiviral therapy to prevent the disease from occurring in the future.
The following symptoms are characteristic of trichomoniasis:
- Itching and burning.
- Copious discharge of a cloudy or greenish color with a foamy consistency.
- Pungent aroma of rotten meat.
- Pain when urinating.
Mycoplasmosis manifests itself:
- Transparent watery discharge with a pungent odor.
- Itching and burning.
- Irritation of the labia.
- Discomfort during intimacy.
- Nagging pain in the lower abdomen.
Ureaplasmosis is characterized by copious clear or cloudy discharge without a distinct specific odor. In this case, the woman begins to be bothered by unpleasant sensations in the genital area, which intensify during sex and urination.
There are many STDs that can cause itching and an increase in vaginal secretions. And here it is important to accurately determine the cause of these symptoms, since further treatment will depend on this. And in order to accurately determine the causative agent of the disease, you will need to submit a vaginal smear for bacterial culture, which is taken by the gynecologist during the examination.
Physiological
The occurrence of unpleasant sensations in the genital area and heavy discharge can occur not only due to the activation of pathogenic flora in the vagina, but also as a result of the influence of certain factors on the body.
Most often, such symptoms are observed in women against the background of an allergic reaction. It can occur on:
- Cosmetics for intimate hygiene.
- Lubricants.
- Sperm from a sexual partner.
- Medicines.
- Gaskets.
- Powders and conditioners.
In this case, solving the problem is quite simple. It is necessary to eliminate the impact of the irritant on the female body, and also take an antihistamine. Sometimes, itching and burning can be caused by insufficient personal hygiene and wearing too tight underwear made from low-quality materials.
In medical practice, there are often cases when women come to the gynecologist with complaints of similar symptoms, but during the examination they do not reveal any pathologies. In such situations, doctors often attribute the patient’s condition to mental disorders. As they say, all diseases come from nerves. And this case is no exception. To solve the problem, a woman needs to take a course of antidepressants and try to protect herself from stress and anxiety. As reviews show, this is enough to eliminate unpleasant symptoms.
White discharge with itching
A woman should pay attention to her condition if she experiences the following white discharge:
- cheesy character;
- foamy;
- scaly;
- with a sharp sour odor;
- with a rotten smell;
- with a fishy smell.
White discharge and itching in the intimate area are symptoms that the following diseases are present in the body:
- thrush;
- bacterial vaginosis;
- Trichomonas colpitis.
Also, in some cases, leucorrhoea and itching in women can also occur due to non-compliance with the rules of intimate hygiene, which causes the rapid proliferation of pathogenic bacteria and fungi, as well as the erosion of tissues by urine residues.
Medications
White discharge in women and itching, the causes of which are determined by the gynecologist, are most often treated with antifungal and antibacterial agents. In rare cases, it is possible to take hormones and antibiotics, which are selected individually for each patient. With thrush, during which women complain of itching in an intimate place inside, the white discharge is quite intense. Doctors usually prescribe the following medications for the disease:
In the case of bacterial diseases, treatment with antiseptic agents such as miramistin, chlorhexiline and a weak solution of manganese is indicated. You should not prescribe medications on your own, since only a gynecologist will be able to determine the cause that caused itching and white discharge in an intimate place.
Yellow discharge
In the case where yellow discharge and itching are noted, the woman can’t even talk about the norm. These phenomena are symptoms of a pathology that must be treated as early as possible. Most often, when yellow discharge accompanied by itching appears, a woman is diagnosed with:
- colpitis,
- adnexitis,
- bacterial vaginitis,
- salpingitis,
- chlamydia,
- trichomoniasis,
- cervical erosion.
Treatment
If you begin to notice that an unpleasant-smelling secretion has been coming out of your vagina for several days, which is accompanied by itching and burning, go to the doctor and get all the necessary tests. After receiving the examination results, the gynecologist will be able to determine the exact cause of these symptoms and prescribe appropriate treatment.
So, if a woman was found to have a cheesy discharge of a grayish or white hue and, after a microscopic examination, she was diagnosed with thrush, then special antifungal drugs in combination with immunomodulators or multivitamins can be used as therapeutic therapy. For inflammatory processes, anti-inflammatory therapy is used, and if infections are detected, broad-spectrum antibiotics are used.
Remember that vaginal discharge can occur for a variety of reasons. Therefore, their treatment must take place individually! All medications are selected in such a way that they not only eliminate the symptoms, but also relieve the patient of the very cause of their appearance. This is the only way to preserve women’s health for many years!
Home remedies
When itching in an intimate place and the white discharge does not have an unpleasant odor, you can use the recommendations of traditional medicine. In such a situation, women need to wash and douche with infusions of chamomile or calendula. They are prepared by pouring 1 tablespoon of raw material into 200 ml of boiling water. Infuse the product for 1 hour under the lid. Treatment is carried out 2 times a day. You can alternate the composition of chamomile and calendula.
Several signs indicate that women's health is in order. The girl does not feel any pain, the menstrual cycle is as accurate as a clock, and the discharge is translucent or whitish in color and has practically no smell. Brown secretion can also be considered normal if this phenomenon occurs a few days before menstruation or immediately after it. If your vagina becomes itchy and brown discharge begins to stain your underwear in the middle of your cycle, this may be a sign that the delicate balance of health is disrupted. Most often, both of these symptoms can be explained by several factors, but sometimes, a single problem is to blame.
Treatment for white curdled discharge due to candidiasis
Thrush is one of the pathological conditions that requires immediate response from the patient and a visit to the doctor. After examination and confirmation of the diagnosis, the gynecologist will definitely take measures aimed at eliminating the symptoms of the disease. Modern methods of treating candidiasis include its drug correction, which is implemented by prescribing antifungal agents.
Recommended drugs
- Clotrimazole suppositories, which are intended for local treatment of candidiasis. Prescribed in a dose of 100 mg daily for 6 days in a row (introduced into the vagina before bedtime).
- Fluconazole (Diflucan) in the form of capsules, vaginal suppositories, solution for intravenous administration. For candidiasis, it is prescribed in a dose of 150 mg once.
- Mifungar cream (Oxiconazole). Apply to damaged skin once a day (before bedtime) for 18-21 days.
- Mikosist. For thrush, take 1 time per course in a dose of 150 ml.
- Pimafucin is an antibiotic from the macrolide class. The product is available in the form of cream, tablets, vaginal suppositories and solution. For vaginal candidiasis, the patient inserts 1 suppository into her vagina at night for 3-6 days.
- Polygynax. It has a powerful antifungal and antimicrobial effect and is available in capsule form. The drug is administered 1 capsule at night for 12 days.
Diet
For thrush, doctors prescribe a special diet to their patients, which enhances the effect of drug therapy, reduces the appearance of odorless, curd-like discharge with itching, and prevents the development of relapses of the disease. Women suffering from candidiasis should exclude the following foods from the daily menu for the entire period of treatment and until the pathological symptoms completely disappear:
- chocolate, cakes and pastries, sweets and other confectionery products;
- alcoholic drinks;
- strong black tea and coffee;
- vinegar and dishes that contain it even in small quantities (marinades, preserves);
- ketchup, mayonnaise and hot sauces;
- blue cheese;
- smoked meats;
- fried and fatty foods prepared with spices and synthetic seasonings (flavor enhancers).
To reduce vaginal itching and odorless yellowish or white cheesy discharge even without taking medications, doctors recommend enriching your diet with foods such as:
- vegetables, in particular beets, carrots, Brussels sprouts and cucumbers;
- stewed fish with vegetables;
- boiled poultry;
- unsweetened fruits, especially lemons;
- berries;
- legumes and grains;
- seaweed;
- seafood;
- cereals;
- natural yoghurts and low-fat cottage cheese.
Brown discharge and itching in women: causes
It is important to observe at what period of the menstrual cycle the discharge of brown secretion from the vagina is observed. So, if a color change appears in the middle, then this indicates that ovulation has begun. During this process, the production of estrogen increases, which affects the walls of the uterus. As a result, blood particles may appear in the secretion. Such spotting should not cause alarm - this is the norm.
Brown discharge with itching appears, sometimes immediately after such situations:
- gynecological examination;
- rough sexual intercourse;
- inaccurate insertion of a tampon.
In such cases, the vaginal mucosa is damaged, which leads to a change in the color of the secretion and a burning sensation in the intimate area. There is no need to worry if both symptoms disappear 3-4 days after the incident.
A hormonal surge is also often the reason for the appearance of secretion of an unusual color and this happens during the period:
- adolescence;
- taking hormonal drugs;
- menopause.
Brown discharge after menstruation and itching have nothing to do with physiology, especially if the latter symptom bothers you constantly and intensely. Let's consider what can be suspected based on the appearance of one or both of these phenomena:
- Cervical erosion. Bleeding does not always appear, but only if the surface of the mucous membrane where there is erosion is damaged.
- Endometriosis. Metrorrhagia appears spontaneously, without any connection to the menstrual cycle, pain may not bother you, and there is no itching.
- Sexually transmitted diseases. Diseases are characterized by the presence of two complaints at once. There is both brown discharge and constant itching of the genitals. This is how trichomoniasis, chlamydia, and syphilis can manifest themselves. An infectious process is also indicated by pain in the lower abdomen, an unpleasant smell of secretions, and pain when urinating.
- Ectopic pregnancy. Almost black discharge can replace menstruation and stain underwear for a long time. Symptoms of normal pregnancy do occur, which should alert both the woman and the doctor.
- Tumors. The nature of the formations can be either benign or malignant. If the process has just begun, then the only symptom may be metrorrhagia, which is not caused by physiology, and subsequently pain and deterioration in general well-being are added.
Details about the norm
Vaginal discharge in women must be present. Their functions:
- protection of the body of the uterus and its cervix from microorganisms that have pathogenic properties;
- sanitation of the genital tract;
- moisturizing the mucous membrane of the genitals - “natural lubrication.”
Normal vaginal discharge includes the following components:
- secretion secreted by glands located on the cervix;
- sweating (transudate) of a small amount of tissue fluid from the vaginal wall;
- “waste” cells of reproductive organs - epithelium, as well as cells of the immune system - leukocytes (the latter in very minute quantities);
- lactobacilli (Dederlein bacilli) and a limited number of other non-pathogenic cocci bacteria.
Discharge in healthy girls under 10 years of age should not be recorded. This is due to a certain hormonal balance and anatomical features of this age. Only when menarche approaches - puberty - is it possible for a mucous discharge to appear, which is supplemented by menstruation a year later. Therefore, the appearance of vaginal discharge, which also “goes in tandem” with one of the signs of the disease (itching, burning) before the age of 12, is a symptom of a disease of either the genitourinary or digestive systems (usually an infection).
The exception is the discharge of whitish mucus on days 2-7 after birth. This is called a “sexual crisis” and develops due to the fact that in the child’s blood there is several times less gestagens that came to him during pregnancy from the mother.
If normal discharge changes color
Cyclic changes in normal secretion
Vaginal discharge in women should have the following characteristics:
- consistency like raw chicken protein;
- light color or colorless, transparent;
- volume per day – 2-4 ml;
- no discomfort, itching or other unpleasant sensations;
- There is no smell at all or it can be described as slightly sour.
Depending on the period of the cycle, vaginal discharge changes, which is normal:
1. Cyclic (menstrual) bleeding - the release of 30-80 ml of blood in 3-7 days. Blood should be a different color on different days of your period.
2. Vaginal secretion after menstruation and before ovulation (until the middle of the cycle) should have the following characteristics:
- not abundant even in young girls (1-2 ml - like a small stain on underwear);
- slimy or watery;
- most often homogeneous, but lumps of mucus up to 2 mm may also occur;
- colorless, less often – whitish or yellowish;
- the smell may be absent and may be defined as slightly sour.
3. Ovulation period:
- increased discharge (up to 4 ml/day);
- the consistency is characterized as viscous, mucous;
- more often – transparent, sometimes can be beige;
- detection of blood streaks is allowed (within a couple of days).
4. Three days after ovulation:
- there is less discharge;
- it is transparent or whitish;
- The consistency ranges from viscous, jelly-like to creamy.
5. A couple of days before the onset of menstruation, the discharge of mucus from the vagina in women may increase again (an optional sign).
Normally, a year before the appearance of menstrual blood, a girl should experience the following mucous discharge:
- liquid (less often - mucous);
- whitish (rarely - with a yellowish tint);
- not accompanied by any discomfort.
After the appearance of cyclic bleeding, leucorrhoea (that is, vaginal discharge in women) will be more abundant for 1-3 years. With the onset of the “peak” of the childbearing period, their total number will decrease. During menopause, the amount of vaginal secretion will gradually decrease again, but not to the point of complete disappearance.
Discharge of a changed color, or even transparent, but accompanied by pain in the area above the pubis or on both sides of it, fever, itching or pain is a pathology.
Vaginal secretion – brown
Secretion of this color in women can occur in the following situations:
- At 12-15 cycles - may indicate the onset of ovulation.
- In women over 40, they talk about atrophic processes in the endometrium (in this case, the discharge is not accompanied by pain or discomfort).
The first two reasons are the norm. More often, the secretion of mucus of this color indicates the development of such pathologies:
- uterine polyps;
- endometriosis;
- genital tract infections (may be accompanied by a feeling of local itching);
- ectopic pregnancy;
- Dysfunctional bleeding due to an imbalance of a woman's hormones.
Thick leucorrhoea
- Transparent and thick discharge is normal during the ovulation period.
- With trichomoniasis, women also develop thick leucorrhoea. They are usually yellowish or green (less often grayish) in color and are usually accompanied by itching.
A large amount of secret
Discharge in women with an increased daily volume may be:
- normally – after sexual intercourse, during sexual arousal;
- as a sign of STDs (mainly trichomoniasis, when there is a lot of leucorrhoea, it is foamy, gray-yellow, thick, accompanied by itching of the vagina and vulva);
- with an imbalance of sex hormones;
- when the walls of the genital organs (vagina or uterus) prolapse due to childbirth or frequent hard physical work;
- as a sign of vaginosis;
- evidence of pathology of any nature in the cervix;
- a consequence of allergies to condoms, underwear, pads, tampons;
- if they are profusely yellow and darken before and after cyclic bleeding, this is a sign of chronic endometritis or endocervicitis.
Mucous and clear discharge
Determined in normal amounts (up to 4 ml/day) are a sign of absolute normality.
A copious secretion that has a transparent base can normally appear after sex and during sexual arousal. It also accompanies some pathologies transmitted through sex and oncological problems of the reproductive organs.
White discharge
Is a sign of the norm:
- on the days of ovulation (lasts 1-3 days),
- after coitus – several hours,
- during pregnancy.
White discharge is also characteristic of candidiasis (most often when the fungus is associated with a virus or pathogenic bacterium), but this disease is characterized by severe itching, pain and burning in the external genitalia.
Leukorrhea (this is what profuse leucorrhoea is called) can also occur with certain infections and with oncological pathology of the reproductive organs.
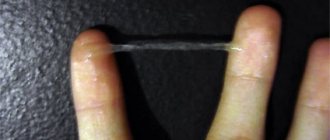
Curd secret
The discharge of flakes in women that resemble cottage cheese and have different shades is characteristic of candidiasis - thrush. Usually, there is significant itching of the vestibule and the vagina itself, as well as the vulva, which is why the woman cannot even work, sit or lie normally. Scratching the inflamed genitals leads to the appearance of a large number of cracks on them, the contact of which with urine causes severe pain (because of this, women try to hold back urination). This is a classic version of thrush, which is now quite rare, due to widespread advertising and the use of antifungal agents by women before receiving the results of a smear.
In some cases, cheesy leucorrhoea, even when accompanied by itching, can indicate:
- urea and mycoplasmosis;
- chlamydia;
- combination of one of the above pathologies with thrush.
Yellow vaginal discharge
Such a complaint indicates that the woman has some kind of infection of the vagina, cervix or uterine body:
- Chlamydia: not only the bright yellow discharge is disturbing, but also pain in the hypogastrium. There is discomfort during urination. The Bartholin gland in the vestibule of the vagina also enlarges.
- Trichomoniasis: the discharge is most often foamy in nature. They are yellowish-green and have an unpleasant odor.
- Gonorrhea: leucorrhoea of a purulent nature, profuse, yellow in color.
Watery vaginal discharge
1. If it is white, it could be:
- after ovulation – a variant of the norm;
- a sign of inflammation of the endocervix, then usually blood streaks are detected in the “water”.
2. Possessing a changed odor:
- chlamydia;
- gonorrhea;
- bacterial infections;
- trichomoniasis.
3. If the discharge in women is brown in color and watery in nature, this indicates:
- endometritis;
- polyp in the uterus.
4. Yellow watery discharge indicates inflammation of the uterine appendages - ovaries or fallopian tubes.
5. Bacterial vaginosis (imbalance of vaginal flora): the discharge has a different color - from gray to yellow-green, and has a “fishy” smell.
Purulent discharge
Pus is released from the genital tract in the event of bacterial inflammation:
- uterus;
- appendages;
- for gonorrhea.
In the last two cases, the woman’s general condition usually suffers: she feels weak, lethargic, nauseous, the temperature rises and severe pain appears in the hypogastrium of the abdomen.
Discharge with altered odor
Almost always, such discharge is a sign of the development of an infectious pathology in the uterus or vagina (any flora can do this), as well as a violation of the vaginal biocenosis (vaginosis). In the latter case, the smell is characterized as that of rotten fish. Bacterial vaginosis is not characterized by itching.
Pink discharge and itching
The acidic environment of the vagina is nature’s idea to protect health from infections and bacteria that can penetrate from the outside. This happens normally, but if conditions change, the pH of the mucous membrane is also disrupted. At this moment, the immune system is not able to fight back against a bacterial attack, which leads to the development of various pathologies, resulting in itching, burning and pink discharge. Also called provoking factors:
- Severe stress. Constant worries negatively affect hormonal levels, which often triggers a whole chain of reactions in the body. This definitely affects women's health.
- Poorly selected intrauterine device.
- Long-term therapy using hormonal drugs for diseases that are in no way related to the reproductive organs.
- Improper functioning of the thyroid gland.
Most often, pink discharge and vaginal itching occur as a result of a combination of several pathologies, for example:
- vaginal dysbiosis and fungal infection;
- endometrial inflammation and chlamydia;
- cervical erosion and chronic diseases of the endocrine glands.
Blood discharge
There are many reasons for this condition. To understand them, it is best to divide them by periods of a woman’s life.
For girls
If blood appears in a child under 10 years of age, this may be evidence of:
- premature maturation of the reproductive system due to endocrinological pathology;
- infection in the genital tract;
- diseases of the kidneys or urinary organs;
- diseases of the digestive system.
For girls
In girls 12-18 years old, a phenomenon such as dysfunctional (also known as juvenile) uterine bleeding is often observed - the release of blood outside the menstrual period.
Juvenile bleeding occurs due to:
- abnormal development of the genitals;
- infections – general and local;
- stress;
- improper nutrition.
In women before menopause
The discharge of any amount of bloody discharge of any color in women 18-45 years old can be caused by the following pathologies:
- endometriosis;
- severe cervical erosion;
- trauma to the vagina or overlying genitals;
- oncological diseases of the genital organs;
- infectious lesions of the genitals;
- chronic endocervicitis, endometriosis;
- endocrinopathies;
- endometrial hyperplasia;
- ectopic pregnancy;
- miscarriage.
Bloody discharge that occurs before or after menstruation can also occur in “non-threatening” situations:
- when taking emergency contraceptives (“Postinor”);
- when taking hormonal contraceptives for the first time;
- within a week after the abortion;
- when canceling COCs;
- after gynecological procedures (even examination using a gynecological speculum).
Discharge during pregnancy
During pregnancy
Here, only one type of blood from the genital tract can be normal - implantation bleeding. This is the release, a week or 9 days before the expected cyclic bleeding, of a small amount of mucus streaked with blood, associated with the introduction of an established embryo into the endometrium.
It is also not dangerous to release non-scarlet blood in a very minute amount and in the form of streaks after examination with the help of mirrors, vaginal ultrasound or sexual intercourse during pregnancy. This usually indicates erosive damage to the cervical epithelium.
All other blood discharge, even if it occurs during the expected period, indicates the following pathology:
- the threat of spontaneous abortion;
- placental abruption;
- frozen pregnancy, when the dead fertilized egg detaches.
After childbirth, the discharge of blood is considered physiological if it persists for 4-6 weeks and passes from the stage of dark blood discharge to a white and yellow leucorrhoea, which is called lochia.
During menopause
After the final cessation of menstruation, bleeding can rarely indicate a pathology other than cancer. Typically, these symptoms include cervical cancer and endometrial cancer.
Treatment of discharge
Treatment of discharge
Treatment for any unusual leucorrhoea should be started after a visual examination by a gynecologist. If we are talking about purulent or bloody discharge, treatment will begin immediately, without waiting for the results of a smear. In other cases, the doctor needs to get an idea of the nature of the inflammation, the type of microbe, and its sensitivity to antimicrobial drugs.
All you can do on your own is make an appointment with a gynecologist (if we are not talking about the discharge of pus or blood, then you should not wait for a scheduled appointment, but go to an appointment with the gynecologist on duty for consultation or call an ambulance) and take a short course of lactobacillus preparations (“Lacidophilus”, “Bio-Gaia”, “Bifilakt”). Everything else should be prescribed by the doctor.
Thus, discharge and vagina exist both normally and in various conditions and diseases. They can characterize a large number of both local and systemic diseases. A gynecologist must determine the cause and prescribe treatment.
Itching and spotting in women
The color of leucorrhoea always reflects the state of women's health. Discharge is of great diagnostic importance, so it is important to monitor not only what color it is, but also note its consistency, smell, and time of appearance. So, when bloody secretion is released from the genital tract, the doctor can diagnose nonspecific vaginitis. This disease occurs in such a way that only discharge can indicate its presence. In addition to the color, the smell also changes, it becomes distinctly unpleasant. Burning and itching are also almost always a concern.
The inflammatory process in the endometrial layer is also accompanied by abundant secretion with the presence of blood or pus. Endometritis often occurs like this:
- body temperature rises;
- leucorrhoea produces an unpleasant odor;
- The lower abdomen hurts and “pulls.”
Sometimes metrorrhagia, as bleeding is also called, can be a sign of pregnancy. Fluid with blood is released due to the attachment of an egg, which has already been fertilized, to the endometrium. You can notice a slight release of reddish secretion 6-7 days before the start of your expected period. For the rest of the period of bearing a child, such bleeding is a reason to go to the hospital without delay.
Curd discharge in women: treatment with folk remedies and methods of modern medicine
The main condition for quick and effective relief from unpleasant symptoms is a timely visit to a specialist for a correct diagnosis. The sooner the gynecologist conducts the necessary research and determines the cause of the discharge, the sooner he will prescribe treatment.
White cheesy discharge in women caused by fungal infections can easily be treated with local antifungal drugs (antimycotics).
- The use of vaginal suppositories, as well as creams and ointments, is common. Local treatment is effective only for mild and acute candidiasis, but if the disease has progressed to the chronic stage, it becomes much more difficult to get rid of it. In such cases, the doctor prescribes tableted antimycotics, sometimes combining them with local medications.
- It is worth noting that white curdled discharge does not always indicate the presence of a fungal disease. Sometimes scanty mucus of off-white or grayish color with a curd-like consistency is possible due to sexually transmitted bacterial diseases. Then the specialist prescribes antibacterial drugs in combination with anti-inflammatory drugs and physiotherapy.
- For pain in the abdominal area, antispasmodics are additionally used. Similar methods of therapy are used for inflammatory processes in the area of the uterus and appendages, in which yellow, curd-like discharge is observed.
- Women with signs of trichomoniasis or gonorrhea need to visit a venereologist together with her sexual partner. Illnesses accompanied by yellow cheesy discharge, burning and a pungent odor are dangerous with serious and irreversible complications. In such cases, the woman and her partner need urgent treatment with antibiotics and a complete cessation of sexual intercourse for a certain period.
- In addition to the main therapy, the gynecologist prescribes symptomatic treatment. So, the patient may be prescribed medications against itching and burning in the vagina. Before treating curdled discharge in women caused by decreased immunity or stress, the doctor will prescribe immunomodulators and vitamin complexes, and sedatives to the patient.
Is it acceptable to treat white or yellow curd discharge with folk recipes?
- In the old days, many improvised means were used to treat curd discharge. Women douched with soda and tanning infusions, irrigated the vaginal area with solutions of garlic and vinegar, took baths with chamomile, or more often took a steam bath. In fact, it is better to refrain from using traditional recipes, as this provokes complications and difficulties in making a diagnosis by a doctor.