First of all, it is necessary to note such a problem as vulvovaginitis - inflammation of the labia. It is provoked by menstruation, natural leucorrhoea, dirty laundry, masturbation, touching the genitals with dirty hands. Vulvovaginitis is manifested by a tickling sensation in the area of the external genitalia, which turns into pain when walking and visiting the toilet. As the disease progresses, the natural discharge acquires a yellow-green tint and an unpleasant odor, and the external genitalia hurt even more.
Why does the vulva hurt?
Gynecologists warn that a woman’s genitals should not hurt under any circumstances. If pain appears, you need to urgently go to the gynecologist.
It is impossible to independently diagnose the disease based on the nature of pain in the labia; one can only assume the cause.
Let's look at a few examples:
- Allergic reaction. Pain in the labia, defined by patients as burning, itching, tingling, is often associated with allergies. The reaction occurs as a result of the use of sensitizing cosmetics, low-quality underwear and panty liners.
- Infection of the genital organs and urinary tract. The pain may be the result of a growing intimate infection, either bacterial or viral. In this case, women complain of red, aching and swollen labia. Burning and pain may increase with urination, which may also indicate a urinary tract infection.
- Vulvar cancer. Pain in the labia may be a sign of cancer. The most important symptoms of cancer are severe itching and pain in the vulva.
- Vulvodynia. Vulvodynia is also one of the reasons. In this case, women are haunted by chronic acute or burning pain, most often in the area of the vaginal vestibule. Upon examination, irritation is detected in the vulva area.
Pain during menstruation
If a woman experiences pain during her period, this may indicate the following problems:
- Vulvodynia, which is characterized by pain in the vulva. The disease has a chronic course. Painful sensations appear when using tampons or during sexual intercourse. This condition is provoked by infections, injuries, chronic diseases of the genital organs, allergic reactions;
- Incorrect choice of tampon size or allergy to the components from which the pads are made;
- If a woman is diagnosed with candidiasis, the labia also itch.
The cause of the labia is varicose veins
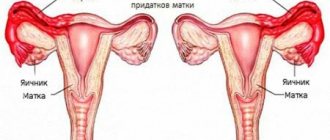
Varicose veins usually appear in pregnant women. The pathology is found to one degree or another in 40% of pregnant women and affects the veins of the lower extremities and anus. The cause of the pathological condition is the pressure of the enlarging uterus on large venous vessels - the inferior vena cava and iliac veins. This causes blood stagnation in the pelvic area, vasodilation, and ultimately the appearance of varicose veins.
Common symptoms of varicose veins include:
- dilated, visible veins in the upper thighs and buttocks, spreading around the periphery;
- hyperalgesia, pain in the vulva and labia;
- hyperemia and swelling of the labia;
- discomfort during sexual intercourse;
- constipation;
- problems with urination.
Other risk factors for developing labial varicose veins include obesity, a sedentary lifestyle, chronic constipation, lack of exercise, and abdominal hypertension.
Diagnosis of the disease is based on ultrasound with Doppler of the pelvic venous vessels. Treatment of varicose veins of the vulva consists of embolization or sclerotherapy of diseased veins, which involves closing the lumen of the vessel. In pregnant women, the disease often goes away on its own a few months after birth.
Causes of pain in the labia area
The labia are bodily folds that perform a barrier and shock-absorbing function. They prevent the penetration of pathogens and foreign objects into the vagina, and also prevent damage to the vagina in the event of a fall or rubbing of the perineum by a bicycle seat, horse saddle, etc. There are two types of labia majora and minora: the first are large skin ridges covered with hair, the second are moist folds hidden under them, penetrated by blood vessels. Both can increase in size and become sensitive due to the following factors:
- blockage of the sebaceous glands, creating the prerequisites for the formation of subcutaneous fatty tumors - wen;
- inflammation of the hair follicles after shaving, hair removal or depilation of the bikini area;
- irritation of the skin resulting from failure to comply with personal hygiene rules, using low-quality tampons or pads, wearing synthetic or lace underwear, riding a bicycle or motorcycle with a hard seat;
- inflammation of the tissues of the vagina or labia;
- varicose veins of the small pelvis;
- inflammation of the lymph nodes caused by an infectious disease or cancer process occurring in the body;
- exacerbation of thrush or herpes as a result of hypothermia, taking antibiotics or frequent use of intimate hygiene products (gel, soap, wet wipes) with antibacterial properties;
- inflammation of the glands, which are located at the entrance to the vagina and produce a mucous secretion that maintains moisture inside the specified element of the reproductive system;
- incorrect functioning of the endocrine system;
- rough sex or invasive diagnostic intervention;
- taking strong medications, such as chemotherapy drugs.
Usually the labia hurt during menstruation, since during this period the sensitivity of the nerve receptors located in the groin area increases, plus blood flows to the labia, which is why they swell and become very susceptible to external influences. If a woman uses pads, and her work involves staying in a sitting position for a long time, then she will experience discomfort in the groin area. As a rule, after the end of menstruation, the unpleasant sensations disappear, so those who are faced with this problem do not rush to see doctors and, in principle, do the right thing: such pains do not require treatment, since their occurrence is due to natural causes.
Soreness of the labia not associated with the onset of menstruation is termed “vulvodynia.”
This pathology manifests itself through:
- itching and burning in the groin area;
- redness and swelling of the labia;
- specific vaginal discharge;
- persistent pain in the lower abdomen.
Vulvodynia develops in women who have injured the lower body, who have not treated an infectious or inflammatory disease in time, or who have suffered severe poisoning. This pathology is treated under the supervision of a gynecologist. If necessary, a gastroenterologist, infectious disease specialist or dermatovenerologist may be involved in the process.
Vulvovaginitis (inflammation of the genitals)
Occurs when the following symptoms appear:
- Swelling of the labia appears, as well as an itchy and uncomfortable condition;
- When moving and urinating, severe pain is felt;
- Irritation and redness are visible on the labia.
The disease can occur as a result of infection due to unwashed hands, mechanical damage to the genitals (friction from poor-quality underwear and tight underwear).
Candidiasis or common thrush
The signs are:
- Inflammatory process inside the vagina;
- The labia become painful and often itch;
- Discomfort appears during and after sex;
- Discharge is visible on the underwear. They have a cheesy appearance, white or yellowish color and a sour odor.
In women, candidiasis leads among other diseases of the reproductive system. This is explained by the fact that the Candida fungus constantly lives in the female body. As a result of a decrease in the protective functions of the body, this fungus begins to actively develop, which leads to a clear manifestation of the disease. Also, the development of candidiasis can be affected by previously untreated chronic infection or unprotected sex.
Vulvodynia
Has the following manifestations:
- There is itching and burning in the genital area;
- Any touch causes pain;
- The vagina is very inflamed.
This disease has similar symptoms to other pathologies and therefore it is important to correctly diagnose it. Vulodynia can form as a result of incorrect/incomplete treatment of candidiasis or due to prolonged use of antibiotics.
Bartholinitis
Characterized by the following:
- Lump on the genitals;
- Severe pain;
- Unpleasant sensations during sexual intercourse.
The inflammatory process occurring in the Bartholin glands provokes swelling of the labia and their soreness. This disease occurs as a result of infection with genococcus and staphylococcus.
Gardnerellosis
Symptoms:
- Vaginal itching and pain;
- Foamy discharge with a fishy odor;
- Problems with urination.
This infection is characterized by sexual transmission, but there are also cases of pathology developing as a result of pregnancy, hormonal disorders, and menopause.
Venereal diseases
The following types are distinguished:
- Chlamydia;
- Ureaplasma;
- Mycoplasmas;
- Genital herpes virus;
- Gardnerellas.
Itching and pain occur as a result of:
- Not maintaining sexual hygiene;
- Using synthetic and tight underwear;
- Not quite the right selection of hygiene products: pads, tampons, intimate area care products;
- Use of medications that cause itching;
- Violation of the vaginal microflora;
- Malfunctions of the endocrine system, stomach, as well as metabolic disorders.
The appearance of itching and pain in the genital area often indicates sexually transmitted and infectious diseases. Self-treatment is not suitable in this case. The first step is to accurately diagnose the cause of unpleasant symptoms.
Pain in the vulva due to infection - vulvitis
Inflammation is one of the most common diseases of the vulva and labia. May have a bacterial, viral or fungal etiology. The most common symptoms of inflammation:
- pain in the vulva and labia;
- burning and itching in the vulva area;
- swelling and redness of the labia;
- Due to itching, scratches form, which only increases the discomfort.
Vulvitis usually occurs as a result of sexually transmitted diseases - gonorrhea, chlamydia, syphilis, venereal ulcers, trichomoniasis and others.
Causes
The following factors can cause pain:
- violation of personal hygiene rules;
- negative reaction of the body to products intended for the care of the intimate area;
- constantly wearing synthetic or tight underwear;
- treatment with drugs that cause such side effects;
- mucosal problems;
- hormonal disbalance;
- infectious diseases;
- venereal diseases;
- psychological problems;
- gynecological problems that appear during or after sex;
- insufficient lubrication during menopause;
- menstrual irregularities.
Vulvar pain and Bartholin gland abscess
Bartholin's glands are large vestibular glands located at the back of the labia minora, right at the entrance to the vagina. They secrete mucus designed to moisturize the vagina. This protects the epithelium from abrasions and irritations.
Sometimes the Bartholin glands can become inflamed. And in case of obstruction and closure of the lumen of the gland, an abscess of the Bartholin gland develops. An abscess is characterized by very severe pain in the vulva, making it difficult to sit.
Pain in the labia does not go away with any painkillers. Relief will only come from cutting the abscess and evacuating the purulent contents by a gynecologist. To prevent the abscess from recurring, the edges of the wall of the open abscess are sutured into the surrounding mucous membrane.
In addition to pain in the labia area, the abscess is accompanied by other symptoms:
- swelling of the labia - usually one-sided, on the side of the abscess;
- redness of the labia;
- noticeable swelling in the area of the abscess.
After surgery you will need to take broad-spectrum antibiotics.
Pain during pregnancy
Pain occurs in the second trimester of pregnancy. This is due to increased blood flow, as a result of which the lips increase in size, pain and swelling occur. This is considered normal if varicose veins are not diagnosed.
The pain goes away on its own after the baby is born. To relieve discomfort during this period, a woman is recommended to take more frequent walks or lie on her side. It is not recommended to stand or sit for long periods of time.
Pain after childbirth
Many women wonder why the labia hurts after childbirth. This is a natural state that should not be feared. During childbirth, when the baby passes through the birth canal, the lips and mucous membranes are injured.
Therefore, large lips often hurt and are swollen. It goes away on its own. The main thing during this period is to carefully observe personal hygiene.
Aching labia and scleroderma
Scleroderma is usually diagnosed in postmenopausal women. It is an atrophic and inflammatory disease of the vulva and labia, leading to scarring and secondary infections of the vulva. Scleroderma is considered a precancerous condition, which without treatment ends in the development of squamous cell carcinoma of the vulva.
Clinical symptoms of vulvar scleroderma are whitish, sometimes pearlescent skin lesions in the genital area. The predominant symptoms of scleroderma are primarily burning and itching. As a result of scratching, wounds are formed and infection may occur. Due to developing inflammation, pain is noted in the labia and vulva.
Treatment of infection involves the use of antibiotic therapy. To stop the process of scleroderma, corticosteroids are selected to reduce inflammation. Surgical treatment is usually not required. Decisive for the success of treatment is a quick visit to a gynecologist when the changes have gone too far.
Share link:
One-sided pain
If the pain radiates only on one side, a woman is most often diagnosed with the following diseases:
- Bartholinitis is when the gland located deep in the lip becomes inflamed. It becomes clogged and its proper functioning stops. Swelling and pain appear;
- Vulvovaginitis is associated with inflammation of the vulva and mucous membranes. The labia hurts, discomfort, itching, burning appear;
- Lip injury;
- Tumors;
- Herpes;
- Varicose veins, when peripheral veins become swollen. Blood circulation is impaired, the mucous membrane dries out, and pain appears on one or both sides.
Symptoms of vulvar pain
Women experience varying degrees of vulvar pain. Its types can be described as follows:
- baking;
- burning;
- stinging;
- annoying;
- cutting;
- tingling;
- pressing;
- pulsating;
- itchy.
The pain can be localized, that is, appear in one place, or generalized, that is, spread to the entire vulva.
Vulvar pain can be triggered by pressure or touch, or it can occur on its own, without any external influence. For some women it appears and subsides, but sometimes it can be permanent.
Home treatments
Several home strategies can be used to reduce vulvar pain in women. They include the following.
- Selective approach to the selection of hygiene products. Sometimes using products that do not cause irritation is enough to minimize vulvar pain. Women suffering from vulvar pain should avoid harsh soaps or untested intimate hygiene gels. In addition, during menstruation it is necessary to use pads and tampons that are based on one hundred percent cotton.
- Refusal to douche. The vagina is self-cleaning, so there is no need to use douching or other types of cleaning. Substances that enter the vagina and external genitalia when douching can cause irritation, especially if a woman suffers from vulvar pain.
- Support from loved ones. Vulvodynia can affect interactions with loved ones, self-esteem, or intimate relationships. In such situations, it is extremely important to enlist support. In Western countries, there are special support groups for people with a variety of conditions, including vulvar pain. In Russia, qualified medical specialists can tell you how to build relationships with partners in the presence of this problem.
- Refusal or minimizing the frequency of wearing tight clothing. Tight-fitting clothing and synthetic fabrics such as spandex or lycra can aggravate vulvar pain.
- Using sitz baths. Taking a hot sitz bath with a teaspoon of Epsom salts can often help relieve irritation.
Treatment for vulvar pain
Treatment of pain will be aimed at eliminating its main cause
Methods for eliminating pain in the external genitalia depend on the reasons that cause this pain. If we are talking about an infection, then, as a rule, medications are prescribed. For hormonal changes, hormone replacement therapy (HRT) is considered the most effective treatment, and in cases of injury, surgery may sometimes be required.
In addition, therapists or physical therapists can often help relax tight muscles and also target treatment to address underlying chronic illnesses and anxiety.
Other treatments include:
- Biofeedback. When we think about biofeedback in the context of vulvar pain, it teaches a woman to relax her pelvic floor muscles and monitor how her body responds to the factors that cause pain.
- Local anesthetics. They are usually prescribed as ointments and applied 20-30 minutes before planned sexual activity. They lead to numbness of certain areas of the vulva, so that the woman does not feel any discomfort.
- Pelvic floor therapy. In some cases, this type of treatment helps relax the pelvic floor muscles, relieving muscle pain and tension. Strengthening these muscles supports and helps relax the pelvic floor organs, including the bladder, uterus, and rectum.
- Nerve block. Nerve blockade may help women who experience pain that interferes with daily activities and are unable to relieve their symptoms with other therapeutic strategies. During this treatment, the doctor introduces special injections into the nerves that connect to the external genitalia, thereby blocking the receptors, relieving pain and discomfort.
Causes of vulvitis
In order to clearly understand the causes of vulvitis, it is worth dividing this disease into 2 types: primary and secondary. Primary vulvitis develops in the case of:
- Failure to comply with the rules of intimate hygiene (irregular washing, rarely changing tampons and pads during menstruation, rarely changing underwear, wearing tight and synthetic underwear).
- Sudden hypothermia or overheating of the body.
- Mechanical damage to the vulvar mucosa during sexual intercourse, constant use of tight clothing made of coarse fabrics, removal of hair, and combing.
- Chemical exposure to various drugs.
- Hormonal imbalance and metabolic disorders (obesity, diabetes, insufficient ovarian function, lack of vitamins and minerals in the body);
- Allergic reactions.
Irritation of the labia can be caused by thrush, colpitis (Vaginitis), endometritis (Endometritis) and other diseases of various organs, not necessarily directly related to the mucous membranes and skin of the genitals.
Inflammation of the labia - vulvitis
As medical statistics show, secondary vulvitis most often occurs in women of reproductive age, while primary inflammation is more often diagnosed in childhood. This is facilitated by the tendency of children to diathesis, helminthiasis (Helminthosis) (pinworms with improper hygiene can get into the labia area, causing an inflammatory process).