Cleaning after a miscarriage is carried out taking into account the doctor’s recommendation. Evacuation of the fetus after a frozen pregnancy and spontaneous miscarriage is carried out with a partial abortion. If there is no bleeding, the woman should undergo an ultrasound. To detect a frozen pregnancy, the expectant mother should visit a gynecologist once every 7-14 days.
How does cleansing work after a miscarriage?
A miscarriage is a spontaneous abortion that occurs due to a number of negative factors. Fetal rejection can occur at different stages. Sometimes the gynecologist notes that the embryo has completely exited the organ and no additional curettage is required. Despite the fact that the uterus can clean itself on its own over the course of two to three weeks, in some cases a procedure is prescribed to remove particles of the embryo from the internal cavity of the organ, which is classified as cleansing. To do this, the doctor uses special instruments to open the cervix, and then scrapes out the surface layer of the internal cavity. The procedure is necessary if spontaneous abortion does not clear the uterus of fetal membranes and particles of the fertilized egg. If bleeding or infection has been diagnosed after a miscarriage, the cleaning procedure is carried out immediately. In other cases, the need for an event is determined only by a doctor after an examination.
Infertility after abortion
Abortion is a great stress for the female body, because the reproductive system was already ready to receive and develop a new life.
An abrupt interruption of processes started by nature often leads to hormonal imbalances and other disorders in the body. The incidence of infertility after abortion largely depends on the method of termination of pregnancy. Most often, various folk methods and methods not certified by the Ministry of Health lead to it. Although the procedures practiced in official medical institutions are less dangerous, complications after them are also possible.
Let's look at what types of abortions there are and why infertility may occur after they are performed.
Pharmabort (medicinal method)
It is carried out during pregnancy up to 6 weeks. The patient is given several tablets that must be taken at a certain interval. The result of their action is spontaneous miscarriage. The method is the least traumatic because it does not require surgical intervention.
The difficulty lies in predicting the reaction of each specific organism to the received dose of drugs. Sometimes fetal rejection is accompanied by severe bleeding, pain and other side effects.
Infertility after this type of abortion can develop if vacuum aspiration of the contents of the uterine cavity is used, when the fetal tissue is not completely released.
Miniabortion (vacuum aspiration)
The method can be used up to 7 weeks of pregnancy. It is carried out by aspirating the fertilized egg along with the embryo from the uterine cavity with a special instrument.
The danger is that particles of the fertilized egg can remain in the uterine cavity and provoke an inflammatory process. As a result, a woman may become infertile due to closure of the fallopian tubes or other pathological changes in the pelvic organs.
During aspiration, the walls of the uterus can also be injured, and scar tissue forms at the site of scratches, which will subsequently interfere with implantation of the embryo.
Curettage (surgical abortion)
It is performed under general anesthesia. It consists of scraping the fetus from the uterine cavity along with the mucous membrane. With this method, the likelihood that particles of fetal tissue will remain in the uterus is minimized.
However, other complications may occur:
- adhesions, due to which the fallopian tubes become obstructed;
- scarring, which can lead to ectopic pregnancy in the future;
- cervical injuries, often leading to miscarriage.
After curettage, the likelihood of infection increases if sufficient personal hygiene is not maintained or sexual activity is resumed too early.
The possibility of infertility exists with any method of abortion, but this does not mean that it will occur in any case.
Negative consequences can be avoided if you follow doctors' recommendations. Preventive measures will be discussed later in this article.
What is the probability of infertility after the first abortion?
The probability is about 10% if the abortion was performed in a certified medical institution, and about 40% if the procedure was performed using traditional methods or in an illegal doctor's office.
From the point of view of preserving a woman’s health, abortions are highly not recommended for the following groups of patients:
– nulliparous;
– have had a previous caesarean section;
– with oncopathologies in the uterus;
– with a pregnancy period of more than 20 weeks.
How to avoid infertility after an abortion
Our experts have selected 8 recommendations that will help prevent infertility after an abortion:
1. It is necessary to undergo an examination by a specialist within 10-14 days after the abortion. The doctor will assess the condition of the uterine cavity, give directions for tests and ultrasound, and, if necessary, prescribe hormonal and anti-inflammatory drugs.
2. Any unpleasant changes in well-being should prompt you to immediately consult a doctor.
3. Excessive exercise and heavy lifting should be avoided for at least two weeks after the abortion.
4. Hypothermia of the body is unacceptable until it has fully recovered.
5. You should abstain from alcohol for a week, especially if you have been prescribed antibiotics.
6. Sexual rest is required for 2-3 weeks.
7. It is undesirable to visit swimming pools and baths during the recovery period; hot baths are also contraindicated.
8. After an abortion, it is imperative to use protection so that a new pregnancy does not occur when the reproductive system is not at all ready for this. Your doctor will advise you on contraceptive methods.
Treatment of infertility after abortion
In some cases, infertility caused by the consequences of an abortion can be cured. It all depends on the nature of the emerging pathology.
If infertility is suspected, a woman will be prescribed a series of examinations. Treatment methods will depend on their results.
Hormonal imbalances are corrected by administering hormone-containing drugs in a certain dosage. They will restore the menstrual cycle and improve the functioning of all endocrine glands in the body.
Inflammatory diseases are usually treated with medications and physiotherapeutic procedures.
Obstruction of the fallopian tubes and scar formations are eliminated surgically, usually by laparoscopic method.
If the cervix is damaged and there is a high probability of premature dilatation, appropriate measures are taken to maintain the pregnancy.
If it is not possible to correct disturbances in the functioning of the systems, they resort to the help of assisted reproductive technologies.
In the “Clinic of Professor A.M. Feskov” highly qualified specialists are always ready to provide individual consultations on the issues of competent pregnancy planning, as well as diagnosis and treatment of infertility.
To make an appointment, please use the online form on the website or by phone: +38 and 0 800 50 77 90.
Source: //sana-med.com.ua/ru/besplodie-posle-aborta.php
Scraping process
Cleaning after a miscarriage is carried out only after a laboratory test of blood clotting - a coagulogram, as well as a general blood test. Additionally, a woman’s body is examined for various infectious diseases. Before scraping, it is necessary to shave off the hair
pubis and do an enema. After the preparatory work, the gynecologist examines the patient, and it is important to determine the shape, size and location of the uterus in the pelvic cavity.
Cleaning after a miscarriage is carried out in the gynecologist's chair. To prevent infection of the organ by bacteria and viruses, an antiseptic treatment of the cervix and vagina is first performed. To scrape out the top layer of the internal cavity of the organ, a special instrument called a curette is used. In some cases, the doctor prescribes vacuum cleaning. The entire top layer must be removed. The procedure is quite painful, so it is performed either under general anesthesia or local anesthesia. The procedure takes approximately 15 - 20 minutes. In order to exclude repeated cleaning, hysteroscopy is additionally performed. After surgery, a woman feels pain in the lower abdomen for several hours to several days. The symptoms of pain are similar to menstruation, so special treatment and pain relief are not used. Immediately after cleaning, heavy bleeding appears. After completion of the intervention, periods can last up to 10 - 14 days. This condition is normal, so there is no need to sound the alarm. The absence of blood after cleaning may indicate its accumulation in the internal cavity. If the girl took any medications before surgery, she must inform the doctor about this. Also, 8 hours before surgery it is forbidden to eat or drink.
Cleaning after an early miscarriage is carried out only if the doctor, as a result of an ultrasound examination, has discovered fragments of the embryo inside the uterine cavity. In some cases, even particles cannot be removed, since the uterus is capable of cleaning the cavity on its own during the menstrual cycle. If the procedure has been prescribed, then it is carried out as usual, scraping out the entire top layer.
What is cleansing in gynecology?
Gynecological cleansing of the uterine cavity is a mini operation that is performed under anesthesia, since the procedure is not pleasant and causes pain. Cleaning the uterus can be of 2 types: therapeutic and diagnostic. Therapeutic cleansing is prescribed for medical reasons.
It's running
:
- During an abortion;
- Ectopic pregnancy;
- Miscarriage;
- Endometritis;
- Uterine fibroids;
- Removal of polyps.
Women are always cleaned only in a good hospital or maternity hospital. Diagnostic cleansing is used when it is precisely necessary to identify the causes of negative symptoms, which indicate that the patient’s reproductive system is not functioning properly. The material collected after diagnosis is sent to the laboratory for examination.
The procedure is performed mainly before menstruation is due to begin.
However, sometimes the procedure can be performed in emergency cases, for example, in case of bleeding. This is required in order not to damage the biorhythm of the women’s body with the intervention. In addition, a procedure such as hysteroscopy is prescribed, which allows the doctor, after completing the manipulations using a hysteroscope, to examine the results of the work. This device also improves control over the specialist’s actions during the operation.
The operation goes like this
:
- It begins with dilatation of the cervix using instruments or medications.
- As soon as the cervical canal is able to pass the curette, the uterine lining is cleaned.
- At the final stage, the dilators are removed, and the entire surgical field is treated with an antiseptic. The doctor selects the drug.
To avoid pain, anesthesia is given. Ice must be placed on the stomach to stop the bleeding. While bleeding occurs, the woman should lie down. When the effects of anesthesia wear off, the patient can begin a normal lifestyle with few physical restrictions. She can go home. But for control, the postoperative period requires the supervision of a doctor, because the cervix will remain slightly open for about 30 days. How long does uterine lavage last? The operation does not take long; in general, the procedure takes no more than half an hour.
Vacuum cleaning
Vacuum cleaning after a miscarriage involves complete cleansing of the uterine cavity from contents. This method is prescribed for a number of reasons:
- cleaning the cavity after the birth process;
- miscarriage;
- embryo frozen in development;
- termination of pregnancy - abortion.
This method is the safest and most effective for cleansing the internal cavity of the organ. During the procedure, all contents are completely removed along with part of the mucous membrane. The need for this method is determined only by a gynecologist. The patient must be hospitalized. The operation is considered physiological, since the upper mucous layer is removed, which is torn away from the organ during the menstrual cycle. The most unpleasant thing about this procedure is the opening of the cervix. To do this, the woman is first given anesthesia, and then a dilator. After opening, the doctor begins aspiration.
Cleaning technique
Cleaning is carried out only after an examination has been carried out - for example, the woman undergoes an ultrasound and laboratory tests to determine if the infection of the body has already begun. Vacuum cleaning is carried out only with local anesthesia, since the procedure does not entail the formation of serious microtraumas.
Regular or postpartum vacuum cleaning of the uterus takes place in the following sequence:
- To begin with, the doctor carries out external and internal treatment of the internal organs - it is important to prevent the penetration of infections and bacteria into the internal organs during the vacuum procedure.
- The doctor then increases the diameter of the cervix, which allows the procedure to be performed under normal visual examination. For enlargement, special instrumental expanders are used.
- After all the preparatory stages, the doctor carries out all the necessary actions to scrape out the remaining clots and particles of the placenta.
As a rule, the procedure itself does not take more than half an hour, although sometimes a woman’s condition can be so aggravated that more time is required for cleaning. A woman does not feel pain during aspiration, but she may be disturbed by the sensations characteristic of curettage, which cause very unpleasant feelings.
Pregnancy after curettage
Cleaning is a procedure that causes both physiological and psychological trauma. Therefore, repeat pregnancy requires special planning. Time should be given to restore both the body and the psychological state. As a rule, doctors allow conception three to six months after surgery. For the possibility of fertilization, the doctor must take into account the following factors:
- Patient's age;
- General health;
- Mental background;
- The rate of recovery of the body;
- Hormonal regime.
All of the above aspects are necessary to take into account pregnancy planning. This is due to the thinning of the endometrial wall after curettage. Therefore, early pregnancy can cause the placenta to form incorrectly and lead to serious complications. The cleansing procedure also injures the cervix. As a result, the holding power of her muscles may weaken and lead to another miscarriage. If a girl becomes pregnant before the permissible period, then she must immediately inform the doctor about it. In this case, special monitoring of the condition of the woman and fetus is required.
Only careful planning of pregnancy will minimize the risks of deterioration in the health of both mother and child.
Rehabilitation after cleaning
Mandatory cleaning requires mandatory rehabilitation time, for whatever reason the procedure would not be applied. During rehabilitation, the woman remains under observation for another 1-2 days. In some cases, the observation time of doctors may increase - after cleaning the uterus in the event of a miscarriage or frozen pregnancy. This is important in order to avoid such dangerous and widespread infection and toxic poisoning of the body.
Rehabilitation after the procedure involves the following actions:
- the woman is prescribed a course of antibacterial drugs to prevent infection and exposure to clots previously present in the uterus;
- additionally, after childbirth, a course of administration of medications to contract the uterus is prescribed;
- if there is a complicated situation, the patient is given internal and external treatment of the genitals with antiseptics and other drugs for better recovery.
After the procedure, the uterus bleeds, since curettage causes partial microtrauma to the walls of the organ. Within a week, heavy bleeding ends, gradually the composition of the discharge becomes less concentrated and with the loss of an unpleasant odor. Already on the 10th day, the discharge ends. In the case of the procedure after childbirth, the discharge also stops earlier by 1-2 weeks - this is due to the removal of the contents of the uterus.
This is important: You should not refuse to stay in the clinic after cleaning, as this can lead to dangerous consequences. The presence of the remains of the placenta and other accumulations in the uterus entails their rapid decomposition, which does not appear immediately - as a result, toxic poisoning of the body may appear after vacuum aspiration.
What is vacuum cleaning of the uterus?
Vacuum cleaning of the uterine cavity (vacuum aspiration) is the removal of its contents along with the upper functional layer of the mucous membrane. For high-quality manipulation, a device called a “vacuum aspirator” is used.
It is a catheter, or aspiration tip, connected by a flexible tube to an aspirator. The mechanism uses a pump to create negative pressure. The powerful suction effect created by the aspirator allows you to collect and remove accumulated blood and particles of the contents of the uterine cavity.
An alternative to the hardware method is manual (manual) vacuum aspiration. It is carried out using a mechanical tube in which negative pressure is created by the force applied by the doctor.
Advantages of using vacuum aspiration:
- Vacuum cleaning is considered a gentle method that minimizes complications in the form of an inflammatory process;
- The cervix and the uterus itself are not injured, or these injuries are minor;
- It is possible to carry out the procedure under local or general anesthesia;
- Vacuum aspiration restores a woman’s reproductive health and the ability to conceive and bear a child without complications in the future.
The procedure is performed in a hospital by an experienced obstetrician-gynecologist. For local anesthesia, injections of analgesics are used, for general anesthesia, intravenous administration of anesthesia drugs is used.
The disadvantage of this method is that all manipulations in the uterine cavity are performed blindly. In addition, in most cases, the material taken cannot be used for detailed histological examination.
Manual examination of the uterine cavity (video)
In general, reviews of the procedure are positive. However, to avoid negative consequences, it would be right to consult a professional doctor. The specialist will determine why the uterus contracts poorly, whether there are any traces of placenta or clots, and will perform high-quality cleaning of the uterus and the necessary examination.
One of the safest methods for removing membranes is vacuum cleaning of the uterus during a frozen pregnancy. It is also considered the most effective in terms of removing an embryo that has stopped forming. Only a narrow list of consequences, complications, and effects of this surgical intervention on the female body is highlighted.
Curettage, performed with the help of a vacuum, has a wide list of indications, among which are the clearing of the tract at the end of labor, after a miscarriage, abortion, and the elimination of a frozen fetus.
Carrying out vacuum aspiration during a frozen pregnancy implies the elimination of everything that is in the uterine cavity. In this case, extraction occurs together with the superficial region of the organ mucosa.
Before aspiration cleaning of a pregnant woman with a frozen fetus, it is necessary to undergo preparation:
- do an ECG;
- conduct a general and biochemical examination by donating blood;
- determine the degree of blood clotting activity;
- undergo an examination to diagnose the presence of hepatitis B, C, syphilitic infection, human immunodeficiency virus;
- undergo oncocytological examination.
The doctor must examine the cervix before the procedure and also find out whether the woman has taken medications that affect the quality of blood clotting.
To minimize the risk of damaging the uterus during surgery, a woman must comply with several restrictions that apply to the preoperative period:
- 14 days before the procedure, you should not take medications that affect blood clotting activity.
- After the operation is scheduled, sexual contact should be avoided.
- It is necessary to abandon the douching procedure.
- On the eve of the manipulation, you should not use cosmetics necessary for intimate hygiene.
- The use of vaginal tablets and suppositories should be avoided.
12 hours before surgery you must stop eating. This limitation will make pain relief more effective and safer.
In what cases is the procedure performed?
Vacuum cleaning is not a frequently prescribed gynecological procedure; serious reasons are needed for its implementation. Indications for vacuum aspiration:
- Frozen pregnancy in the early stages of fetal development (up to 12 weeks);
- Spontaneous termination of pregnancy with incomplete removal of particles of the fertilized egg;
- Incomplete delivery of the placenta after natural childbirth or after cesarean section;
- Taking a sample of the internal contents of the uterus for microscopic or bacteriological examination;
- Accumulation of blood in the uterus (hematometra);
- Planned early termination of pregnancy (medical abortion);
- Hydatidiform mole (growth of chorionic villi in the form of bubbles with liquid);
- Volumetric bleeding from the uterus.
Indications for the procedure
By cleaning the uterus with a vacuum, you can remove all the insides of the organ along with its upper mucous layer. There are several indications for this procedure:
- bubble skid;
- a serious disease in the embryo that was diagnosed before the 12th week;
- hematometer;
- spontaneous incomplete miscarriage;
- the presence of placental remnants after childbirth or cesarean section;
- heavy bleeding;
- fetal freezing;
- examination of the uterine microflora for the presence of possible infections that threaten the life of the child.
How is the cleaning done?
To carry out the procedure, the woman sits on a gynecological chair. If the uterus is cleaned after childbirth, then the manipulation is carried out directly on the birth table.
Local or general anesthesia is required for vacuum aspiration, which involves forced dilation of the cervix, as this is the most painful part of the procedure. Postpartum cleansing in most cases is performed without anesthesia, since the cervix during this period has a sufficient degree of dilation.
Sequence:
- The vaginal walls and cervix are fixed using dilators;
- The genitals are treated with an aseptic solution;
- Anesthetic injections are performed into the cervix and periuterine tissue; for general anesthesia, preference is given to intravenous anesthetic drugs;
- The doctor inserts a speculum into the vagina to monitor the progress of the operation, opens and dilates the cervix, if necessary;
- The gynecologist uses a special probe to measure the distance from the entrance to the cervix to its fundus in order to calculate how far the aspirator catheter can be immersed;
- An aspiration tube is inserted into the uterus and a vacuum is created in it;
- The gynecologist fixes the aspirator tip in one position or rotates it to collect the desired material.
After a period of time determined by the doctor, the woman needs an ultrasound examination of the uterine cavity to monitor the condition of this organ. If the study shows that there is no blood, placenta or fertilized egg inside the organ, then the cleansing was successful.
Features of vacuum aspiration in various conditions:
Vacuum cleaning of the uterine cavity after childbirth.
If there are placenta particles, blood clots, and other atypical tissues in the uterus, it will not be able to fully contract after childbirth. After an ultrasound confirming the atypical condition of this organ, medications that contract the uterus or manual cleaning may be prescribed.
If these methods are ineffective, the woman in labor is prescribed vacuum cleaning. After aspiration, she takes antibiotics to prevent inflammation, and the woman undergoes antiseptic treatment of her reproductive organs. Breastfeeding will have to be stopped for the period of treatment, saving milk by expressing.
Vacuum cleaning of the uterine cavity during a frozen pregnancy or hydatidiform mole.
Fetal death may result in spontaneous abortion. If it remains in the uterus, sooner or later its decomposition begins, which leads to intoxication of the female body, to sepsis. Vacuum aspiration allows you to get rid of particles of the fertilized egg and placenta that were not exfoliated when the dead embryo was released.
With a hydatidiform mole, the contents of the uterus cannot be expelled spontaneously. Bubbles with liquid remain inside the organ and cause the development of a malignant tumor.
If a woman experiences hyperthermia after the procedure, careful examination is required to ensure complete removal of the foreign tissue. After cleaning, the woman must be prescribed a course of treatment with antibacterial drugs.
Vacuum cleaning of the uterine cavity after miscarriage.
The manipulation is carried out to remove placental particles after the loss of an embryo older than 13 weeks, or during a miscarriage between 6 and 12 weeks, when there is a possibility that blood clots and particles of the fertilized egg remain in the uterus.
Here, a wait-and-see approach is more often used, and cleaning is prescribed for severe bleeding and signs of acute infection.
Early termination of pregnancy is performed by aspiration of the contents of the uterus along with the embryo. The procedure greatly reduces the trauma and negative consequences for women’s health inherent in the traditional method.
Possible complications
In most cases, women tolerate the procedure of vacuum cleaning of the uterus well. Unpleasant consequences are rare. Therefore, the method is safe and highly effective.
In rare cases, the following unpleasant manifestations may occur:
- hormonal imbalances;
- incomplete abortion, when the fetus (entirely or part of it) remains intact, pregnancy continues;
- pain in the lower abdomen (painkillers will help);
- inflammation of the genital organs (this is indicated by discharge that has an unpleasant odor);
- the occurrence of defects in the cavity or cervix;
- air embolism (blockage of blood vessels with air) with a fatal outcome. Today this happens in isolated cases, because doctors very carefully carry out manipulations in the uterine cavity.
To avoid possible complications after the procedure of vacuum cleaning of the uterus, you need to do an ultrasound to confirm the complete removal of tissue debris from the uterine cavity. If in doubt, you can consult another doctor.
You should consult a doctor as soon as possible if you have the following symptoms:
- the temperature does not stay above 38° for a long time;
- the discharge with blood is very strong (you need to change the pad more often than every 2 hours);
- spotting is accompanied by an unpleasant odor and does not stop for more than two weeks; the pain in the lower abdomen does not go away even when taking strong painkillers.
Any delay, even with one symptom, is very dangerous. It's not worth risking your health. Only a doctor can determine the cause of the symptoms and take corrective measures.
Note that vacuum manipulations can be prescribed for different purposes in the treatment and diagnosis of diseases of the reproductive organ of various types. There are also other methods, but today this procedure is the most effective and gentle method for the female body. The procedure has been so improved that negative consequences may occur in isolated cases. To eliminate the possibility of complications after vacuum cleaning, you need to carefully listen to any signals from the body. If even the slightest deviation occurs, you should quickly consult your doctor.
A woman’s uterus is often subjected to various instrumental influences, since it is the main reproductive organ of people - men and women. Vacuum cleaning after childbirth
in most cases it saves a woman’s health. If we talk about other cases, cleaning is often the only way to save a life. Therefore, there is no reason to hesitate and think about performing curettage - doctors prescribe such cleaning only in extreme cases.
Vacuum aspiration is the removal of clots and other accumulations in the cavity of a woman’s organ without damaging the cervix and its walls. Aspiration is often a complication after childbirth - this is due to the lack of natural release of the placenta and fetal tissue. It should also be mentioned that independent removal of the contents of the uterus during pregnancy may become impossible due to medical error. Doctors categorically cannot leave everything as presented - this is dangerous for the general health of the woman.
Aspiration is not as dangerous and unpleasant as it seems at first glance, therefore it is strictly forbidden for a woman to refuse it, especially after childbirth. If the doctor prescribes vacuum cleaning, you should not panic - just study all the features of the operation, which are presented later in the article.
Recovery after vacuum aspiration
Many women referred for vacuum aspiration are interested in how much blood flows after the procedure. Since the inside of the uterus is a wound after cleaning, there will still be discharge.
They may look like ichor or blood. Bloody discharge will last from 3-5 to 10-14 days. They are not very abundant and do not have an unpleasant odor.
If the bleeding intensifies, spasmodic severe pain appears in the lower abdomen, you should immediately seek medical help.
The menstrual cycle will improve in 35-43 days, because restoration of the endometrium begins to occur from the first day after aspiration. After the procedure, vaginal tampons cannot be used; the use of sanitary pads is permitted.
Complications after the procedure
Despite the safety of the vacuum procedure, the procedure is a complex gynecological operation, so complications may also develop here.
Such troubles include the following complications:
- perforation of parts of the uterus - formation or mechanical damage to the walls or cervix of the reproductive organ;
- heavy blood loss;
- emerging hormonal and endocrine disorders;
- disruption of the menstrual cycle;
- infectious infection of the genital organs;
- formation of adhesions;
- development of inflammatory processes;
- fusion of the tissues of the wall of the reproductive organ;
- the occurrence of causes contributing to infertility.
The most basic and common complications include injury to the cervix, which increases the risk of developing an isthmic-cervical canal. This pathology negatively affects subsequent pregnancies - there is a danger of premature termination of pregnancy or childbirth. In this case, the woman has to undergo suturing of the cervix - suturing ensures the safety of fetal development.
This is important: Unfortunately, doctors cannot accurately determine the risks of complications even with a full study of the pathology and a high-quality procedure. Due to this factor, it is better to seek medical help only in medical institutions with qualified medical personnel. It is also important to contact the clinic in time if you notice pain in the lower abdomen.
Vacuum cleaning of the uterus is a necessary procedure designed to prevent or eliminate toxic damage to the woman’s body. The procedure is most common after childbirth, but there are cases that force doctors to use instrumental cleaning to preserve the integrity of the reproductive organ, as well as the life of the sick woman. You should not refuse to carry out the procedure, no matter how unpleasant it may be - this provides reliable protection against toxic damage to the body due to the decomposition process that has begun. Unfortunately, doctors cite very disappointing statistics of deaths of women who did not seek medical help in time in the current dangerous situation. Young mothers should be reassured - after giving birth, women are in the maternity hospital under the supervision of specialists, so this is impossible for this to happen to them. Vacuum aspiration is performed immediately when indications are detected.
Nowadays, cleaning the uterus of a woman is prescribed quite often. Almost always, this type of operation causes fear, panic attacks, and unreasonable worries in a woman. The negative condition is associated with many different rumors that circulate about this type of surgery in gynecology, which is prescribed to cleanse the uterus from an unplanned pregnancy or from medical pathologies. Fear is a consequence of ignorance of what this gynecological procedure is. This is an operation, which is otherwise called curettage of the uterine cavity and is prescribed for many medical reasons, and we will talk about this in more detail.
Some practical tips for women preparing for vacuum cleaning
Since vacuum aspiration is a full-fledged surgical procedure, an examination is carried out before the procedure. It includes the standard diagnostic minimum:
- Blood test for infections: HIV, hepatitis, syphilis;
- Determination of blood group and Rh factor;
- General and biochemical blood test;
- Coagulogram (determination of blood clotting);
- Vaginal smear cytology analysis (PAP test);
- ECG.
Immediately before aspiration, 6-8 hours before, you should not eat or drink , as otherwise complications will arise during anesthesia. For complete antiseptics, before the procedure you need to remove hair in the genital area and take a shower.
It is advisable to inform your doctor in advance about possible allergic reactions to medications.
Vacuum aspiration is a reliable method that avoids complications. At the current level of medical development, it does not have serious consequences for a woman’s reproductive function.
Cleaning after a caesarean section
The rules of conduct for a woman in labor after cleansing include taking her health seriously and following the advice of the attending doctor.
- Means and methods for treating the vagina;
- Prohibition on the use of vaginal tampons;
- Ban on douching.
You should temporarily avoid taking very hot baths. It is not recommended to go to the bathhouse and sauna. Doctors also advise avoiding excessive physical activity (lifting heavy loads, fitness). It is also prohibited to have sexual intercourse - vaginal intercourse can cause the development of repeated uterine blood flow or infection in the woman’s genitals.
To eliminate large stagnation of contents in the main female organ, any antispasmodic drug can be prescribed for a short course.
Attention! If a woman takes No-shpa, Papaverine, and any other similar medicine, then breastfeeding is prohibited. This is done because otherwise there will be a toxic effect of this group of medications on the baby’s body.
The duration of medication is always prescribed by the doctor - to assess the woman’s condition, follow-up examinations are used, with a mandatory ultrasound of the pelvic organs. When recovery is underway, the doctor may prescribe light exercises to train the uterus. After a cesarean section, an inspection of the uterine cavity is carried out to make sure that the placenta has come out and not a single piece of the placenta remains in the organ of the reproductive system. All this will help avoid any complications.
Why the fetus freezes during pregnancy: reasons
There are a number of risk factors that can contribute to the cessation of embryo development, which leads to its death.
Let's consider the main reasons that gynecologists identify:
- frequent stress;
- genetic disorders in fetal development;
- active sexual life in the early stages;
- use of potent drugs;
- infectious diseases;
- hormonal imbalance;
- difficult working conditions;
- diabetes.
Causes of fading
There are many reasons that cause pregnancy to fail. This condition can be caused by:
- genetic diseases of the embryo; bladder
- exacerbation of infectious diseases leading to the death of the fetus, which are manifested by the presence of vaginal discharge of a yellowish, greenish, brownish tint;
- ectopic pregnancy;
- hormonal imbalances;
- carrying out several abortions before pregnancy;
- taking certain medications;
- bad habits.
These factors can cause pregnancy to fail at any stage. Other reasons for the cessation of fetal development differ depending on the trimester.
If the embryo has stopped developing for any of these reasons, a vacuum abortion or termination of pregnancy must be performed. And after the procedure, you should undergo the examination necessary to diagnose the condition.
Cleaning the uterus
Frozen pregnancy is not a rare occurrence. According to the observations of specialists, in 10% of all cases the fetus dies for one reason or another. After making an accurate diagnosis, the doctor must promptly rid the uterine cavity of the dead embryo.
Vacuum aspiration in the early stages: consequences and features
Vacuum cleaning during a frozen pregnancy is carried out exclusively in the early stages. Mostly up to 12 weeks. The procedure does not pose any serious threats or consequences. It is performed under general or local anesthesia.
- On a gynecological chair, the patient, undressed from the waist down, is given anesthesia to eliminate pain.
- The genitals are disinfected.
- The obstetrician inserts a speculum into the vagina.
- An aspiration tube connected to an electric aspirator is inserted into the uterine cavity.
- Under the influence of a vacuum, the fertilized egg will be torn away from the uterine cavity and brought out.
- This completes the procedure.
The consequences of vacuum aspiration are gentle surgical curettage. However, consequences are possible.
Advantages of the method and procedure progress
Among the main advantages of vacuum cleaning of the uterus are the following:
- minimal risk of injury to the cervix of the reproductive organ;
- the operation is characterized by simplicity and short duration of time, it can be carried out in laboratory conditions;
- in case of termination of pregnancy using this method in the early stages, hormonal changes in the body can be reduced;
- Menstruation begins within 40-43 days after cleansing the uterus.
If there is a frozen pregnancy, a mandatory termination is required to prevent poisoning of the female body with toxins and to eliminate inflammatory processes, which are caused by fetal disintegration. Vacuum cleaning has proven highly effective in such cases.
Cleaning the uterus using this method can be carried out in two ways: manual (manual) and hardware. In practice, the first version of the reproductive organ in women is more often used, which includes the following stages:
- treatment of the external genitalia with a disinfectant solution;
- insertion of a special speculum into the vagina;
- preparing the cervix for cleaning;
- measuring the distance to the uterine cavity using a special probe;
- insertion of a suction tube;
- the doctor rotates the tube, eliminating tissue debris from the inner shell, or takes the required material for diagnostics.
How does curettage occur: does it hurt?
Before cleaning the uterine cavity, the patient must pass the prescribed tests to exclude possible complications that may arise during the operation.
The intervention will be carried out in a gynecological office under general anesthesia, so there is no pain at all.
- The woman takes off the lower part of her clothes and sits on the gynecological chair.
- Anesthesia is injected into the vein and after the medicine begins to take effect, the doctor installs a dilator in the vagina.
- The genital organs (both internal and external) are disinfected with a special solution.
- A substance is injected that promotes contraction of the uterus to shed the mucous layer of the uterus (endometrium) and simplify the procedure itself.
- A curette (surgical spoon for curettage) is inserted into the dilated canal of the uterus, with the help of which the uterus is cleaned of the dead fetus and the upper layer of the endometrium.
- After removing the biological material, the doctor will take out the instrument and take the patient to the room so that she can recover from anesthesia.
IPF – Institute of Family Planning
Artificial termination of pregnancy in medicine is called vacuum aspiration or mini-abortion. Vacuum aspiration began to be practiced in the 60s of the last century and to this day it is successfully practiced in clinics and gynecological departments.
A mini-abortion is performed at 5-6 weeks by suctioning out the fertilized egg by creating negative pressure. Thanks to vacuum aspiration, it was possible to significantly reduce damage to the uterus, infections, and bleeding.
The popularity of vacuum aspiration is explained by the ability to carry out the procedure on an outpatient basis using simple medical equipment, without general anesthesia, because the procedure is practically painless.
Types of vacuum aspiration
Today, clinics and gynecological departments carry out two types of procedures:
- manual (manual) vacuum aspiration;
- machine vacuum aspiration.
Until what period can a vacuum abortion be performed?
When contacting a gynecologist with a request for a mini-abortion, the gynecologist is first of all interested in the number of days of delay in menstruation (that is, the number of days during which menstruation did not occur).
A mini-abortion can be performed only if there is a delay of up to 21 days, but the best option is to carry out the procedure on the 14-15th day of absence of menstruation, since when performing vacuum aspiration before two weeks there is a risk of not noticing the fertilized egg and removing it.
To have surgery later increases the risk of complications.
Indications for mini-abortion
There are no special indications for a mini-abortion; the leading and sufficient indication is the woman’s desire to terminate the pregnancy. But there are also medical indications for early termination of pregnancy. Vacuum aspiration is indicated:
- during frozen pregnancy;
- with anembryonia;
- if bearing a fetus poses a threat to a woman’s health and life (diabetes mellitus, severe liver and kidney pathologies, malignant tumors, etc.);
- with rubella, influenza and other infections during pregnancy;
- social indications (for rape, being in prison, etc.);
- if necessary, endometrial biopsy;
- if remnants of the fertilized egg are found in the uterus after a pharmacological or surgical abortion;
- when parts of the placenta are retained after childbirth or cesarean section;
- for menstrual irregularities (bleeding);
- with accumulation of blood (hematometra) or serous fluid (serozometra) in the uterine cavity;
- with incomplete spontaneous abortion.
Contraindications for the procedure
Vacuum aspiration or mini-abortion belongs to the group of invasive interventions; in fact, it is a minor surgical operation. Therefore, a mini-abortion has contraindications, as does surgical termination of pregnancy.
Gynecologists call contraindications to vacuum aspiration:
- ectopic pregnancy;
- fever;
- infectious processes of any localization (including “colds” on the lips - herpes);
- acute chronic diseases of organs located in the pelvis or their exacerbation;
- blood clotting disorder;
- less than six months after the previous termination of pregnancy.
Mini-abortion is not performed due to specific contraindications:
- when the pregnancy is more than 5 weeks (according to ultrasound readings);
- with malformations of the uterus;
- for tumors of the uterus, due to which its cavity is deformed.
How is vacuum aspiration performed?
The procedure for performing a vacuum abortion is based on the use of an electric vacuum pump in the operation to extract the fertilized egg from the uterus. Using a pump, a uniform negative pressure is created in the uterus, as a result - the fertilized egg is peeled off from the walls of the uterus and sucked out.
The vessels of the uterus are not damaged during vacuum aspiration, and avoiding the use of metal dilators allows one to avoid trauma to the uterus, which reduces the likelihood of developing cervical insufficiency, which in the future may prevent childbearing.
Preparation period
Before the procedure, the woman visits a gynecologist. During the consultation, the doctor decides on a mini-abortion, finds out the duration of pregnancy, and prescribes a number of tests. The patient is sent for research:
- for sexually transmitted diseases;
- flora smears;
- blood analysis;
- coagulogram;
- Ultrasound.
Before performing the procedure, the gynecologist makes sure that there are no indications, including the absence of a genital tract infection.
At the first stage of the operation, the external genitalia are treated with an antiseptic. Access to the uterus is provided by gynecological speculum.
The cervix is treated with a disinfectant, and sometimes the patient is given local anesthesia, although most often it is done without it.
A catheter is inserted into the uterine cavity with slow rotational movements. Under the influence of negative pressure created by a vacuum apparatus, the contents of the uterus are exfoliated and expelled.
Benefits of the procedure
The main advantage of the procedure:
- the possibility of carrying it out on an outpatient basis;
- absence of cervical injuries;
- rapid restoration of uterine tissue and healing;
- slight deviations in hormonal levels and menstrual cycle.
After an abortion
The entire vacuum aspiration procedure takes no more than 5 minutes. After a mini-abortion, the patient should rest for several hours within the walls of the medical institution.
The gynecologist will give a prescribed course of antibiotics to prevent infections, and in case of severe cramping pain, painkillers.
If there are no complications, the woman can return to normal activities the next day.
To prevent complications after a mini-abortion, doctors recommend:
- abstain from sexual activity for a month;
- avoid heavy physical exertion and hypothermia;
- refuse saunas, steam baths and swimming pools;
- You can’t take hot baths after a mini-abortion, only warm showers;
- maintain genital hygiene;
- take antibacterial drugs to prevent infectious complications;
- take hormonal contraceptives to restore hormonal levels and exclude pregnancy.
2-3 weeks after the mini-abortion, you need to see a gynecologist and undergo an ultrasound. If necessary, the doctor will order tests.
Vacuum abortion: consequences and possible complications
Vacuum aspiration, according to doctors, is the safest operation, since there is minimal risk of injury when performing it. Nevertheless, even after vacuum aspiration complications can arise.
Doctors call possible complications during vacuum aspiration:
- perforation of the cervix or body of the uterus;
- incomplete aspiration after removal of the fertilized egg;
- inflammation of the genital organs;
- hormonal disorders;
- menstrual irregularities;
- secondary infertility.
Menstruation after vacuum aspiration
On days 3-5 after the intervention, a woman may experience bleeding similar to menstrual discharge.
//www.youtube.com/watch?v=v0nsbMcCk8g
But this discharge is not menstruation - this discharge after surgery is associated with hormonal changes in the female body.
IMPORTANT INFORMATION
Real menstruation after a mini-abortion will appear in about a month. In this case, periods may be shorter and more abundant, which is associated with suppression of ovarian function. The menstrual cycle that follows will not differ from the regular monthly cycle.
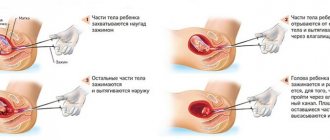
What to do in case of late pregnancy miscarriage
From 9 to 42 weeks of pregnancy, the cessation of fetal development is called antenatal or intrauterine fetal mortality. In the later stages, an abortion is performed. The doctor induces labor artificially.
- A puncture of the amniotic sac is performed and amniotic fluid is removed.
- Next, the patient is given antiprogesterone (Mifepristone) and prostaglandins. Over time, the medications cause contractions.
- The cervix dilates and the fetus comes out.
- In the second trimester, artificial birth occurs without difficulty, since the fetus is still small.
It all ends with curettage of the uterine cavity under general anesthesia. This part of the procedure is mandatory, since the immature placenta may not completely detach from the uterus.
How is the procedure carried out?
The operation is performed under anesthesia to prevent the woman from experiencing pain. The absence of anesthesia is allowed only after childbirth, when the cervix is dilated and the organ is dilated.
After anesthesia is administered, the intimate area is disinfected, the cervix is dilated, and then surgery is performed.
There are several ways to carry out this procedure:
- Manual cleaning. This is done using a special syringe. This method involves suctioning out the contents of the uterus, causing the embryo to tear off. The process is regulated by the doctor himself.
- Machine cleaning. It involves the use of a special pump to extract the fetus.
The procedure lasts no more than a quarter of an hour. Additionally, we recommend that you familiarize yourself with information about the intricacies of its implementation.
Recovery and rehabilitation
A frozen pregnancy brings a woman not only physical, but also psychological trauma.
The expectant mother will have to get used to the thought of losing her child for a long time. Therefore, at first, immediate relatives should provide support and care. Recovery of the body after the procedure will depend on the normalization of menstruation. A healthy lifestyle and proper nutrition will be the best rehabilitation after anesthesia. One of the most important aspects of rehabilitation is the restoration of the endometrium (the mucous membrane of the uterine body). After curettage, an inflammatory process of the mucous layer often occurs. Treatment consists of taking hormonal drugs.
When can you get pregnant again?
It is believed that as soon as the menstrual cycle is restored, the couple can begin to plan for the next pregnancy.
Your period will return in 30-50 days. In order to bear and give birth to a strong and healthy child, for the first 6 months after cleansing, a woman will need to take oral contraceptives, which will help normalize hormonal balance.
The rehabilitation period also includes personal hygiene, which will help normalize the vaginal microflora, and avoidance of physical activity. During the first few months, a woman should be less nervous, move more and eat right to enrich the body with useful substances.
Curettage is a necessary procedure after a frozen pregnancy. Under no circumstances should you avoid it, because it is dangerous not only for health, but also for life. When planning a new pregnancy, you should not be afraid that the pathology will recur. Regular visits to the doctor, taking prescribed medications and getting tests will reduce the likelihood of fetal freezing.
Rehabilitation and possible complications
After the curettage of the frozen fetus is completed, the woman should monitor her body temperature and the nature of her vaginal symptoms twice a day for 14 days. After the specified period, you need to see your doctor in order to undergo examinations after the first frozen pregnancy.
The first step is an ultrasound. This is necessary in order to know for sure that there are no fetal remains left in the uterine cavity.
In addition, tests are prescribed after a frozen pregnancy:
- hormonal examinations;
- diagnostics of the state of microflora, the presence of infectious lesions of the reproductive system;
- study of the histology of the epithelial uterine area.
Such studies will help minimize the risk of fading in the baby’s development during the next pregnancy.
Also during the rehabilitation period, a woman needs to take vitamins and minerals. This is required to strengthen the body. The doctor may also prescribe a course of antibiotics to reduce the likelihood of developing an inflammatory process. Hormonal drugs are recommended to restore background and prevent pregnancy.
It is not recommended to plan a new pregnancy within six months after curettage. This is due to the fact that the female body is weakened during this period, the embryo may again stop developing. You should also avoid sexual relations for a month after the operation. Sexual activity should begin only when the menstrual cycle is restored.
Consequences
After vacuum cleaning during a frozen pregnancy, there is a possibility of complications. Among them are:
- The occurrence of severe pain in the lower abdomen.
- Formation of adhesions.
- The appearance of ruptures in the uterine wall.
- Temperature rises to 37.5 degrees within 1–2 days after surgery.
- The occurrence of inflammation due to damage to the walls of the uterus during incomplete curettage.
- The appearance of bleeding within 6–9 days after surgery. If they are abundant, in order to avoid the formation of blood clots and the development of anemia, you must urgently consult a doctor.
- Infection due to non-compliance with hygiene standards and doctors’ recommendations.
- Hormonal disbalance.
Also, when disinfecting the intimate area, a woman may experience an individual reaction to the applied product. Because of this, cracks appear on the labia and dryness inside the vagina.
Inflammation
One of the consequences of vacuum cleaning is the occurrence of an inflammatory process. This is possible when cleaning a frozen pregnancy not only in the early stages, but also in the later stages.
This complication occurs due to the attachment of infection to damaged tissues. The likelihood of pathologies increases after cleansing, since during this period the immune system weakens and the ability to neutralize pathogens is lost. If a woman does not receive timely treatment for a developing disease, inflammation can progress and affect the ovaries.
Discharge
After vacuum cleaning, various discharges are observed. In the first 6–9 days, bleeding appears, which is similar in nature to menstruation. If it is very strong and lasts more than 10 days, this indicates a pathology that should be urgently eliminated.
After the specified period, bleeding ends. A woman develops a spotting, which normally should not be accompanied by any other color shades or unpleasant odor.
Usually recovers within 30–40 days. If after this period a woman does not have her period, she needs to see a gynecologist. This is due to the fact that such a condition may indicate the presence of a hormonal imbalance, the formation of blood clots that interfere with the separation of blood, and the development of dangerous pathologies that threaten health.