To resolve the issue of family planning, the vast majority of women choose oral contraception. The drugs representing this group of contraceptives are artificially synthesized hormones. They cause changes in hormonal balance, replacing the natural hormonal environment of the female body.
Accordingly, these drugs begin to independently control the menstrual cycle. What changes in menstruation may occur while taking oral contraceptives? More about this.
What does scanty discharge mean?
Poor regulation, with a brown tint, a thicker consistency of discharge instead of menstruation, indicate certain changes in the body. There may also be physiological reasons, such as stress, physical strain, climate change.
Also, spotting may appear while taking oral contraceptives. Most often, this condition is observed in the first months of using OCs or after a long break. Less often, scanty discharge of an abnormal shade indicates serious pathologies - infectious processes, the development of ectopic pregnancy.
Dark brown menstruation (spotting) may be a sign of pregnancy. This phenomenon is sometimes observed from the first month of delay for a period of about 3-4 weeks.
But in any case, it is necessary to figure out why brown discharge occurs instead of standard periods, especially if this repeats from month to month and is accompanied by certain symptoms - pain in the lower abdomen, periodic increases in temperature.
The main causes of brown discharge
If any unusual discharge appears instead of menstruation, it is necessary to carry out a diagnosis. If a woman is planning a pregnancy and does not use protection during sexual intercourse, spotting may indicate conception. But even in this case, it is necessary to find out the reasons for its appearance.
The causes of hypomenorrhea can be more varied: hormonal imbalance, including when taking contraceptives and abnormalities in the thyroid gland, metabolic disorders, inflammation in the genitals.
Long-term use of COCs
Even the most modern contraceptive drugs, to one degree or another, cause hormonal imbalance in women. Oral contraceptives (OCs) contain progesterone and estrogen. A minimal dose of these hormones, penetrating into the blood, can cause a change in the color and volume of menstruation.
Brown spotting instead of menstruation may appear due to the ability of drugs to reduce the formation of the endometrium. Accordingly, menstruation becomes darker in color and its volume decreases. Due to the decrease in the amount of endometrium, a barrier is created for the egg. In addition to thinning the outer layer of the uterus, OCs lead to a decrease in the ovulation period and thickening of the mucus in the fallopian tubes. In combination, this not only makes fertilization of the egg impossible, but also affects menstruation.
Scanty brown discharge may appear for the following reasons:
- incorrectly selected dosage of the active hormone in the selected drug;
- uncontrolled or irregular intake of OCs;
- incorrectly selected contraceptive drug;
- development of side effects while taking oral contraceptives;
- pregnancy or hormonal imbalance after medications.
In the first few months of taking hormonal contraceptives, undesirable consequences are possible, such as a change in the duration of the cycle, a slight delay, and a deterioration in general well-being. This is due to the fact that the reproductive system adapts to the regular intake of progesterone and estrogen into the body. During this same period, thick, rich discharge may appear - not abundant, with a brown tint, the structure of coffee grounds. But if these phenomena do not disappear within six months, you need to contact a specialist.
Pregnancy
Typically, brown spotting is observed in many women in the early stages of pregnancy.
Changes occur against the background of hormonal changes for the following reasons:
- Tissue remaining inside the uterus that did not come out during the last menstruation. They may come out at the beginning of your next period. Due to their long stay in the body, they acquire a rich brown tint.
- Taking oral contraceptives after conception.
- The onset of ovulation. This is evidenced by brown discharge that appears after the end of menstruation. Ovulatory bleeding is observed in every eighth representative of the fairer sex and is considered a normal condition of the female body.
- Increased uterine tone. Light brown discharge instead of menstruation during pregnancy may appear due to intense contractions of the organ, causing endometrial detachment. When leaving the body, it acquires a brown tint.
- The presence of various diseases of the reproductive system, for example, endometriosis.
If there is pregnancy at the time when the first menstruation should have started, various types of spotting, including a brownish tint, may also be observed. The causes of this condition are considered:
- the first signs of a woman’s hormonal changes;
- taking hormone-containing medications prescribed by a doctor as part of therapy to maintain pregnancy;
- the period when the fertilized egg attaches to the uterus. Short-term thick discharge also often appears.
A pathological situation is when spotting appears repeatedly in the first 6–8 weeks of pregnancy.
Under the influence of an increase in the concentration of progesterone, the woman’s body retains the attached fertilized egg. If the level of this hormone is reduced, discharge may indicate a threat of miscarriage and impaired fetal development.
Menstruation while taking birth control pills
To resolve the issue of family planning, the vast majority of women choose oral contraception. The drugs representing this group of contraceptives are artificially synthesized hormones. They cause changes in hormonal balance, replacing the natural hormonal environment of the female body.
Accordingly, these drugs begin to independently control the menstrual cycle. What changes in menstruation may occur while taking oral contraceptives? More about this.
Influence
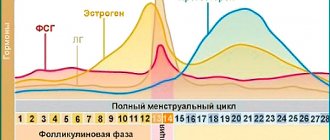
Hormonal contraceptive drugs affect ovulation, blocking or delaying it, and also change the thickness of the endometrial layer (inner uterine lining), thereby preventing conception.
The main effect should include suppression of ovulation. The growth and maturation of follicles does not occur, the egg does not leave the ovary, therefore, fertilization and pregnancy are impossible.
All other effects on the body are considered additional. Oral contraceptives thicken cervical mucus. Thereby creating an insurmountable barrier for sperm penetration.
Due to the effects of OCs (oral contraceptives), the endometrium remains thin, becoming an obstacle to the implantation of the fertilized egg. The contractility of the fallopian tubes decreases, which means the likelihood of an egg passing into the uterine cavity decreases. It is thanks to this complex action of OK drugs that changes in the menstrual cycle are possible.
Changes in menstrual discharge are considered normal during the first three months from the moment you start taking oral contraceptives. The body undergoes a restructuring, it learns to exist and function in new conditions.
If the drug is selected correctly and the administration method is not violated, then after an adaptation period, menstruation will again become cyclical. They will begin regularly at a certain time and end after 3-5 days.
Adaptation
Starting to take contraception may cause light spotting that is not associated with menstruation. That is, spotting appears in the middle of the menstrual cycle. This picture can last from 3 months to six months. Spotting may appear once a month or 2-3 times.
Often, in the first month of taking OK, heavy periods may begin. This phenomenon is called “breakthrough bleeding”, and is a symptom of hormonal imbalance during the adaptation period.
After three months of body restructuring, menstruation becomes regular. They will follow the 21/7 schedule. If the blister contains 21 tablets, then menstruation should begin after the last tablet (usually 3-4 days after the last dose of the drug). If you plan to take OCs continuously, then you should expect your period while taking pacifier pills (placebo).
When taking birth control pills for more than 3 months, scanty periods may occur. This is a normal phenomenon when taking OCs.
In addition, the pain syndrome that often accompanies menstruation disappears.
A positive factor should also include the fact that due to a decrease in the amount of blood released in women, there is an increase in the level of hemoglobin in the blood. This means that the symptoms of anemia disappear.
Changes
Often, after starting to take contraceptives, women experience changes in the nature of their menstrual discharge. They may become abundant, scarce, or disappear altogether.
Scarce
As mentioned above, the appearance of scanty periods is a normal phenomenon when taking oral contraceptives. It is important not to confuse this type of menstruation with the appearance of spotting. If after 3 months the spotting continues, then you should think about choosing another drug. Perhaps the drug was chosen incorrectly or does not cope with its functions.
Bleeding
If very scanty periods when taking OCs occur in the middle of the cycle, and last longer than 3-5 months from the start of taking the drug, then it is worth visiting a gynecologist to change the contraceptive.
If spotting appears at the beginning or middle of the blister with the drug, then this is a signal of a lack of estrogen in the OC; it must be replaced with drugs with a higher dose of this hormone.
If a spot appears in the middle or towards the end of the blister with the drug, this indicates an insufficient amount of gestagen. It makes sense to replace the drug with another one, with a higher dose of this hormone.
Sometimes this kind of daub is an individual reaction to taking OK. In this case, you should choose a different method of protection against unwanted pregnancy or switch to three-phase contraceptives.
Heavy discharge
Often women complain of heavy periods while taking birth control pills. The reasons for this phenomenon:
- Failure to comply with the drug dosage regimen. Perhaps a dose of the drug was missed, or 2 tablets were taken at the same time. This disrupts hormonal levels, causing heavy menstruation.
- Taking the drug provoked vomiting or loose stools, which became an obstacle to the absorption of the active substances of the drug. Hormonal imbalance appears again.
- Taking medications that are not compatible with oral contraceptives. For each OK drug, the list of incompatible drugs is described in detail in the instructions.
- Bad habits, namely smoking and alcoholism, become an obstacle to the absorption and production of the hormone estrogen.
- Diseases of the reproductive organs.
The appearance of heavy menstruation while taking OCs is a reason to immediately contact a gynecologist.
You should not give up birth control if you experience heavy menstruation. Since this will negatively affect the general condition of the body, causing even more heavy bleeding. Hormonal medications should be discontinued gradually, especially if a woman has been taking the pills for several years.
After the condition has normalized, or better yet, during heavy menstruation, you need to visit a gynecologist. Because the reason for heavy periods must be clarified. You may need to replace the drug with another one. Most often, heavy bleeding occurs when taking mini-pills (microdosed drugs). When replacing them with low-dose contraceptives, the woman’s condition normalizes.
No discharge
If, after finishing taking the drug (blister of 21 OK), menstruation has not begun within 7 days, it is necessary to check for pregnancy. To do this, you need to purchase 2-3 pregnancy tests from different manufacturers. If no test shows pregnancy, then you should continue taking the OC according to the usual regimen.
If at least one test is positive, you should contact a gynecologist to confirm the presence of pregnancy. You should stop taking contraceptives during this period.
Unfortunately, the use of hormonal contraceptives does not guarantee 100% protection against unwanted pregnancy. The level of protection is influenced by adherence to the exact time and regimen of taking the drug, the presence of bad habits, and the correct choice of OC. Missing the time of taking a contraceptive by at least one to two hours increases the likelihood of pregnancy.
Statistics show that taking OCs has no effect on fetal development. Therefore, if pregnancy occurs, you can safely register and give birth.
Sometimes, after starting to take OK, periods may be absent for about 3 months. This falls into the norm; the period of restructuring of the body affects it. However, it would be a good idea to carry out pregnancy tests.
If there are no menstruation periods for more than six months, you should consult a gynecologist. Because this condition indicates violations of the reproductive organs.
Recommendations
The most appropriate OC drugs can be prescribed by a specialist after a complete examination of the patient. A mandatory factor is the study of hormonal balance. If contraceptives are prescribed after examining the body, then bleeding or other side effects should not occur.
However, very often the drugs are prescribed without examination, or the woman chooses OK on her own, on the advice of friends or commercials. In this case, the occurrence of intermenstrual spotting and bleeding is almost guaranteed.
There are special criteria that will help assess the correctness of the prescribed drugs. The predominance of one or another sex hormone determines a woman’s appearance.
Women of the estrogenic type. Women of this type are of short or medium height, correctly built, very feminine, with well-developed breasts. They have a deep, enchanting voice with very “feminine” intonations. Their hair growth is of the female type.
The premenstrual mood is nervous, there is engorgement of the mammary glands, and the periods themselves last from 5 days and are characterized by abundance. The menstrual cycle is more than 28 days. Pregnancy proceeds without any problems. Women of this type are shown drugs with an enhanced gestagenic component: Miniziston, Regividon, Microgenon, and so on.
Women of balanced type. Representatives of the fair sex of this type are usually of average height. They have a feminine voice and appearance. The chest is medium size, well developed. Female pattern hair growth.
Premenstrual mood is balanced, menstruation is moderate and lasts no more than 5 days. The menstrual cycle is 28 days. Pregnancy proceeds without complications. Prescribed: Novinet, Logest, Lindinet-20, Lindinet-30, Regulon, Femoden and others.
Women of the progesterone type. They are distinguished by their tall stature, boyish build, and poorly developed breasts. The voice is low, sometimes hoarse. Male pattern hair, skin prone to acne.
The premenstrual state is depressive, the menstruation itself is scanty and lasts less than 5 days. The menstrual cycle lasts less than 28 days. Pregnancy is difficult and accompanied by toxicosis. Prescribed drugs with antiandrogenic properties: Yarina, Jess, Janine, Midiana and others.
There is a group of contraindications for taking OK:
- Oncological neoplasms of the mammary glands and reproductive organs.
- Migraine.
- Thromboembolism.
- Vascular pathologies of the brain.
- Vaginal bleeding of unknown etiology.
- Hereditary hyperlipidemia.
Prescribe with caution in the following conditions:
- High blood pressure (hypertension).
- Epileptic seizures and epilepsy.
- Diabetes.
- Depressive states.
- Pathologies of the liver and gall bladder.
- Absence of menstruation or scanty menstruation in women who have not given birth.
- Having bad habits, namely smoking.
- Women over 40 years of age.
While taking oral contraceptives, you must regularly visit the gynecological office. It is necessary to notify your doctor if you are taking other medications that were prescribed by other specialists (for example, antibiotics), or if you have any symptoms associated with taking OCs.
It is important to know that herbal treatments (such as St. John's wort) may reduce the effectiveness of birth control. Therefore, before starting herbal treatment, it is necessary to consult a specialist and carefully study the instructions for the OC.
If it is not possible to cancel or avoid herbal treatment, then during this period it is necessary to use additional contraceptives (condoms, spermicides and other means).
You need to know that after stopping OC medications, there is a very high probability of pregnancy in the first three months. If pregnancy is not planned, then it is necessary to use additional contraception. It is best to use condoms.
Source: https://uterus2.ru/disease/menstrual-irregularities/otsutstvie-mesyachnyh-pri-prieme-protivozachatochnyh.html
How many days can you wait for normal periods?
When brown spotting is observed instead of menstruation, this may be a variant of the norm depending on the individual characteristics of the body, if menstruation immediately begins with small brown discharge - a sign of conception or ovulation.
But in some cases, spotting indicates pathology, especially in combination with the following symptoms:
- There are any deviations in a woman’s condition: sharp, cutting or aching pain in the lower abdomen, in the sacral area, pain in the lower back, in the side. Along with spotting, such symptoms may indicate the development of an ectopic pregnancy, gynecological diseases, benign or malignant neoplasms in the reproductive system.
- Abrupt cessation of menstruation. On the second day of menstruation after normal bleeding, spotting is also not physiological. She may be talking about hormonal imbalance or ectopic pregnancy.
- The presence of bloody discharge with an unpleasant odor is an inflammation of a bacterial or viral nature, candidiasis. A particularly dangerous symptom in such cases is the smell of rotten fish. It indicates infection by pathogenic bacteria.
The norm is the appearance of scanty menstruation on the first, maximum second day of menstruation. If the regulations continue to not normalize, you should consult a doctor. Also, brown spotting should be a reason to visit a gynecologist if pregnancy is suspected or confirmed.
Menstruation after stopping birth control pills: possible problems
Changes in a woman’s body can be caused by even minor interference with endocrine functions. The reproductive system is no exception.
Menstruation after discontinuation of OCs often comes with a delay in medical practice. This failure is caused by natural and pathogenic factors.
Only a qualified doctor can figure out what led to menstrual irregularities after stopping oral contraceptives.
What should your period be like after stopping OK?
In the first two months after stopping taking hormonal contraceptives, minimal deviations are observed. In rare cases, a rapid return of unpleasant symptoms may occur.
Recovery of the cycle after stopping OK lasts up to three, maximum four months. Often, menstruation is accompanied by the same pain sensations that existed before starting to take oral contraceptives. The headache reappears, sudden mood swings and irritability are observed.
In cases where scanty periods are observed while taking hormonal contraceptives, heavy discharge can be expected no earlier than a month after stopping taking the OC. If the use of birth control pills does not affect the amount of blood during menstruation, there is only a slight increase after discontinuation.
Menstruation may occur a few days after birth control if the woman does not finish the package she started. The discharge is scanty and brown. The duration of such menstruation is about two weeks. Changes occur due to sudden changes in the level of hormones in the blood.
Signs of pathological menstruation
Minor bleeding begins a few days after stopping taking the OC and lasts about seven, maximum fourteen days. Such changes in the body are called withdrawal syndrome.
The reason for a visit to the gynecologist should be heavy discharge during this period, accompanied by pronounced pain and weakness.
The first cycle after discontinuation of OK should begin within one, maximum three months. If there is no menstruation for a longer period, a doctor's consultation is necessary. A delay may indicate the development of various pathologies that cannot be identified independently.
Scanty or excessively heavy discharge during the period of stabilization of the cycle is considered normal, but if after several months the situation does not change, you need to be examined by a gynecologist. Such abnormalities may indicate serious health problems.
Delayed menstruation
The absence of menstruation after stopping OC is considered normal. The duration of the recovery process can be up to three months. If the cycle does not stabilize after six months, you need to conduct a full examination and identify the problem.
In many ways, the timing at which menstruation should begin depends on factors such as:
- type of oral contraceptives and duration of their use;
- age;
- body condition and history of gynecological diseases.
The cycle is restored faster in young girls, but in women approaching menopause, it may not stabilize at all. In case of suppressed immunity, it will take about six months to normalize the functions of the ovaries.
The reason for the absence of menstruation when you stop taking OCs may be pregnancy. It has been proven that the chances of fertilization in women who have previously taken contraceptives are much higher than those who have not used these drugs.
Very heavy periods
After one, and sometimes two months, the first menstruation appears after OK. Due to the fact that while taking the drug, the discharge was scanty, during this period it can become abundant. This is due to hormonal imbalance.
Excessively heavy periods can lead to anemia, as the amount of blood lost increases significantly. In this case, there is a deterioration in the general condition, weakness and dizziness. During this period, it is recommended to start taking medications that contain iron.
In cases where the appearance of heavy bleeding was preceded by a delay, there is no cause for concern. In a short time the cycle stabilizes. You should consult a gynecologist only when such menstruation bothers you for a long time. There is a risk of bleeding.
Scanty and short periods
In most cases, after completing the use of OK, the cycle becomes stable. Violations are observed only in those women who have previously had irregular, scanty menstrual flow.
It is considered normal when, a few days after stopping contraceptives, the first menstruation arrives, characterized by scarcity. This is not menstruation, but signs of withdrawal syndrome - the body’s reaction to hormonal changes.
In addition, the cause of scanty discharge may be:
- pregnancy;
- prolonged absence of menstruation;
- genitourinary system infections;
- polycystic disease;
- cancerous formations.
To exclude the development of pathologies, it is recommended to undergo examination by a gynecologist.
Period more than 7 days
The first period after birth control often lasts more than a week. This process should not cause concern in women and is considered normal, but only if the discharge is scanty and not accompanied by severe pain.
If you find clots in your menstrual blood or your general condition worsens, you should go to a gynecologist to prevent bleeding.
Causes of menstrual cycle failure after discontinuation of OK
Your periods after taking birth control pills may be irregular, scanty, or excessively heavy. Women often experience a delay. This is due to the fact that the body is recovering - and against the background of this, a disruption of the cycle is observed. There may be several reasons for the failure:
- Hormone imbalance. After stopping taking contraceptives, the body is forced to independently produce substances that it previously received through OCs. It takes about three, maximum five months for the hormonal system to recover.
- Pregnancy. A delay after stopping birth control often indicates that a woman will soon become a mother.
- Polycystic ovary syndrome. Changes in hormonal levels caused by the action of contraceptives can lead to the formation of multiple cysts.
- Functional disorders of the endocrine system. Disruptions in the natural production of hormones can cause amenorrhea - the complete absence of discharge.
- Infectious diseases. The menstrual cycle may not be restored for a long time due to the penetration of infections into the body and the development of pathology.
When should you make an appointment with a gynecologist?
After stopping oral contraception, your cycle should return within three months. You need to seek help from a gynecologist in cases where there is heavy discharge accompanied by pain.
The absence of menstruation within three months after stopping taking the pills should cause concern. Perhaps, due to hormonal imbalance, a serious disease has developed that cannot be cured without the help of a doctor.
Cancellation of contraceptives is a strong stress for the body. For this reason, irregularities in the menstrual cycle are observed, and a number of complications cannot be ruled out. Accordingly, women need to devote more time to their health and, if unpleasant symptoms appear, contact a gynecologist.
Source: https://TopGinekolog.ru/menstruation/menstrual-cycle/pri-otmene-protivozachatochnyh-tabletok
What to do in this situation
A woman should contact her gynecologist if any unusual discharge instead of menstruation occurs more than once, appears during pregnancy, is accompanied by pain or discomfort, or is observed between periods. This will eliminate serious pathologies.
To determine the cause, a number of diagnostic measures are carried out:
- External examination of the vagina and genital organs will make it possible to exclude the presence of polyps, erosions and other neoplasms.
- Determination of hCG level. If you had unprotected sexual intercourse before your menstruation, you need to do a test to rule out pregnancy, including ectopic pregnancy. A more reliable result will be obtained from a laboratory study, which can be done before the delay begins.
- Colposcopic examination of the cervix - allows you to determine the location of bleeding ulcers, exclude or detect inflammation on the internal mucous membrane.
- Ultrasound of the fallopian tubes and uterine cavity - detection of hyperplasia, neoplasms, including malignant ones, exclusion of cysts and polyps, additional examination of the mucous membrane. Transvaginal ultrasound, used to detect pathologies in the early stages, and ultrasound examination of the abdominal cavity may also be required.
- General urine and blood tests. With their help, the presence of infectious agents and hormonal disorders are detected in the body. In addition, they indirectly indicate the presence of viral or bacterial inflammation.