Brief information
When a doctor talks about multifollicular ovaries, he does not mean a disease. Strictly speaking, such a condition is not pathological. More often we have to talk about the effect than about the cause.
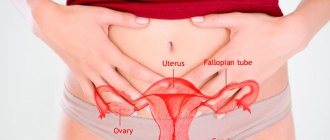
In gynecology, this term refers to a sign of polycystic anatomical structures (multi-cystic ovaries). However, this is not always the case. The ovaries are one of the most important organs of the female reproductive system. Every month, several follicles mature in the structure of the paired organ (their number varies from 2 to 5-6). They contain eggs. As the process progresses, one or a pair of follicles become dominant (their size is more pronounced compared to other follicles). The capsule ruptures and the egg is released into the birth canal (fallopian tube). This cycle is called ovulation.
If doctors note that the ovaries are multifollicular, in practice this means the appearance of a larger number of follicles (over 8-10). In some cases, this may be a variant of the norm, but more often it is a secondary sign of concomitant pathologies and conditions.
Probable Causes
Often, the multifollicular structure of the ovaries is due to subjective reasons - the woman herself becomes the culprit of the condition. Among the likely factors:
- Use of oral contraceptives. Hormonal pills cause inhibition of normal follicle maturation. The absence of menstruation appears. In this case, the structures remain in an immature state: they are not large and developed enough to independently collapse with the release of the egg. As a result, they remain within the ovaries and, when ovulation begins, are noted along with new follicles. This is false multifollicular ovarian syndrome. There is no need to treat it.
- The diagnosis of multifollicular ovaries can be made during lactation. In the period before childbirth and during breastfeeding (immediately after childbirth), the pituitary gland produces large amounts of the hormone prolactin. This substance stimulates milk synthesis, menstruation is suppressed. Accordingly, as in the previous case, the number of follicular structures becomes larger.
- Hypopituitarism. The reasons may be endocrine. As a result of insufficient production of pituitary substances, small follicles accumulate in the tissues of the paired genital organ.
- Burdened heredity. Multifollicular changes in the ovaries are inherited. In this case, we are talking about a physiological norm.
- Significant fluctuations in body weight. With sudden weight loss, the production of the female hormone estrogen slows down. The regularity of menstruation is disrupted.
- Puberty period. Typically, multifollicular changes in the organ occur at the height of puberty. A similar condition occurs in girls under the age of 18. There is no reason to worry. This is a natural transformation of the developing organism. At the end of puberty, the problem will disappear on its own.
- Prolonged psycho-emotional stress. Against the background of prolonged stress and psycho-emotional tension, estrogen synthesis decreases. Normal ovulation stops.
- Multicystic ovarian disease is the only pathological factor among all those described. We are talking about a pathogenic process during which cavities filled with exudate are formed in the stroma of the paired genital organ.
- Multicystic ovarian disease inhibits the normal menstrual cycle.
Causes of multifollicular ovaries
Multifollicularity is most often determined at the genetic level; this condition may be caused by a decrease in the level of luteinizing hormone (LH hormone). Often this hormone decreases with sudden weight fluctuations . This condition may not manifest itself clinically, but sometimes a woman may be bothered by a cycle disorder in the form of irregular (usually rare) menstruation or absence of menstruation for 6 or more months, which can lead to non-pregnancy. This is due to the fact that when the ovaries are multifollicular, there is no ovulation and hormonal levels change. However, multifollicular ovaries can be considered normal, since this condition can also be caused by the woman’s age. This phenomenon is quite often observed in young girls when the formation of the genital organs is completed.
Clinical picture
Signs of a multifollicular ovary are not specific enough. In the vast majority of cases, the problem is discovered by chance, during an examination for another disease. Signs of mfd are disguised as symptoms of other diseases. The clinical picture consists of the following manifestations:
- menstrual irregularities. It becomes irregular, delays are observed;
- long-term inability to conceive. Sometimes a paradoxical situation arises. Menstruation continues, but the woman cannot become pregnant. This can happen when the multifollicular structure of the ovaries is noted.
Multifollicular ovaries and delay are interrelated phenomena. The cycle, as already said, may remain normal, but will extend over a longer period. The onset of menstruation is delayed by 5-7 days (delay), the cycle itself lasts one and a half to two months.
In the absence of pathological processes in the body, this is where the signs end. But, if the root cause lies in polycystic disease or a multicystic process, the clinical picture becomes much brighter. First, you need to understand what it is, multicystic ovarian disease and how it is related to polycystic disease and the diagnosis described.
Polycystic disease is not an entirely accurate name. It is the pathology closest to multifollicular ovaries. However, it is significantly different. As a result of the flow, the paired organs increase in size, and multiple immature follicles are formed in the stroma (more than 10-15, as opposed to 8-10 with multifollicular changes). However, they are significantly larger in size than normal follicular structures. Thus, polycystic disease is close in morphological characteristics to the condition under consideration.
Multicystic disease is a completely different pathology. If in the case of polycystic disease the space-occupying formations are still the same follicles, then with the multicystic process true cysts develop, i.e. cavities filled with exudate. Such terminological confusion complicates the understanding of the essence of pathological changes by ordinary patients. However, distinguishing one condition from another is not difficult when it comes to objective research.
All of the conditions described above inhibit reproductive function and lead to the formation of the following symptoms of complicated multifollicular ovaries:
- pathological body hair of the male type. The so-called hirsutism.
- growth of coarse hair in the genital area, nipples, chin, etc.
- the condition is also characterized by such a manifestation as a change in the body according to the male type. The vocal cords grow and thicken (accordingly, the voice becomes lower), and the volume of muscle mass increases. This is due to a decrease in estrogen production and an increase in the synthesis of testosterone and androgens.
- increased sebum production. Externally they appear as intense acne.
- obesity. Also according to the male type. Lipid structures are deposited on the abdomen and chest area. A body type known as an apple (typical of males) develops.
- multifollicular paired organs are characterized by spontaneous uterine bleeding and painful menstruation.
Small follicular ovaries can present with a variety of symptoms. However, this is not axiomatic. It all depends on the original factor that caused the problem.
Multifollicular ovaries and pregnancy
Often, the presence of MFN does not prevent pregnancy, since these changes do not affect ovulation. Women with echoviral MFN without hormonal disturbances are considered healthy and have a low risk of developing pregnancy and related problems.
However, given the current hormonal dysfunction, that is, the absence of luteinizing hormone, the number of ovulation cycles decreases. As a rule, after proper pharmacotherapy, hormonal disorders are eliminated and problems with pregnancy are eliminated.
If the patient plans to conceive a child after an ultrasound scan, and the result indicates the presence of multifollicular ovaries, then a laboratory study of the hormonal function of the ovaries is recommended.
With polycystic ovary syndrome, pregnancy is unlikely. Almost all (85%) patients with this diagnosis have anovulation and primary infertility, and rare (3-5%) spontaneous pregnancies show premature birth and miscarriages.
Unlike polycystic diseases, in multifollicular ovaries sometimes there are problems with conception, and not with the pregnancy itself. If the result of structural changes in the ovaries has already been taken during pregnancy, a detailed laboratory examination is carried out to identify possible hormonal imbalances for immediate correction.
Progesterone deficiency is the cause of lack of pregnancy
The most common cause of pregnancy anxiety in MFJ is progesterone deficiency. During the formation of the placenta, progesterone is secreted by the corpus luteum during pregnancy. Once the placenta is fully formed, it retains saren to maintain looseness in the corpus luteum and begins to synthesize only progesterone.
The developing and growing fetus is perceived by the uterus as a “foreign body”, which tends to reflexively rupture. Progesterone prevents premature miscarriage by preventing the muscle wall from contracting during pregnancy. It also stimulates the growth of the uterus and is involved in preparing the mammary glands for lactation.
With progesterone deficiency in multifollicular ovaries, there is a risk of premature termination of pregnancy. Despite the possibility of complications, the vast majority of cases of MFJ do not affect the normal course of pregnancy and the fetus.
The state of multiple follicular structures and pregnancy
Girls often wonder whether it is possible to get pregnant with multifollicular ovaries.
Depending on the root cause of the phenomenon, the answer may be positive or negative. Pregnancy with multifollicular ovaries is quite possible if menstruation continues. In this case, dominant follicles are still formed, the eggs are released into the fallopian tube, and fertilization is likely. It is much worse if the cycle is interrupted. In this case, there can be no talk of conception. Relative infertility occurs, which needs to be corrected with medication.
Signs of multifollicular ovaries
Manifestations of multifollicular ovarian syndrome :
- Anovulatory cycles – can occur up to 5 times a year. Their causes are either non-ripening of the dominant follicle or the appearance of a follicular cyst. The absence of ovulation should be confirmed by the result of folliculometry, and not be a woman’s conclusion based on maintaining a BT schedule and using ovulation tests.
- Infertility is a consequence of frequent anovulatory cycles. However, in the case of MFN, it is enough for spouses to use an ultrasound to catch the moment when ovulation occurs and make attempts to conceive. Whereas with PCOS, such tactics would not help - polycystic disease causes a constant absence of ovulation.
- Irregular menstruation is a consequence of improper functioning of the ovaries, as a result of which the first phase of the cycle becomes long, and instead of the required 12-14 days it stretches for 30-40 days. Then the second phase begins, which for multifollicular ovaries lasts, on average, 8 - 10 days. Thus, it turns out that a woman’s menstrual cycle with MFN often stretches for 40–50 days.
How to get pregnant if there is no ovulation
Many patients diagnosed with multifollicular ovaries need to know whether the long-awaited pregnancy will occur or not. You should not think about IVF, it is a pointless waste of money and time. Fertilization may occur, but miscarriage is very likely. The activities are aimed at solving two problems:
- normalization of hormonal levels.
- stimulation of ovulation in multifollicular ovaries.
The set of measures involves completing a full course of treatment. What events are held are described below.
Diagnosis of multifollicular paired gonads
Patients are examined by gynecologists or gynecologist-endocrinologists (preferred). At the initial appointment, an oral interview and medical history are taken. Of great importance in the examination is the establishment of the fact of the inability to conceive and menstrual irregularities.
The main diagnostic method is ultrasound examination of the paired organ. During ultrasound examinations, a diagnostician can identify the described physiological condition. The multifollicular right ovary and the multifollicular left ovary usually look identical with rare exceptions. The right ovary is considered more active than the left, therefore the number of small follicular structures in it may be greater. For this reason, damage to the left ovary is less common.
On ultrasound, the condition is manifested by the following visual signs:
- the size of the anatomical structures is significantly larger than normal. The enlargement of the paired organ is due to hyperfunction and accumulation of follicles in the stroma.
- echosigns of multifollicular ovaries are less intense compared to the echogenicity of the uterus.
- the echostructure of the dominant follicle is indistinguishable in density. Small follicular structures have a similar capsule thickness, which cannot be called normal.
- as noted, more often the problem is found on the right.
- the location of the follicles is peripheral (diffuse).
These are just the main indicators. Interpretation of ultrasound results is the prerogative of the doctor. The echographic “portrait” of the patient is quite typical; there are no problems with diagnosis. As a result of the same ultrasound examination, the diagnostician can detect cystic inclusions in the stroma of the organ. If the described condition is observed in conjunction with a change in the menstrual cycle, the diagnosis becomes obvious.
Therapy for multifollicular ovaries
Strictly speaking, there is no need to treat multifollicular ovaries; it is not a disease or pathology. If there is normal menstruation, there is no discomfort or health problems, nothing needs to be done. It's another matter when there is no ovulation. In this case, drug correction of the pathology is necessary. Treatment of multifollicular ovaries involves taking the following medications:
- hormonal analogues of progesterone.
- drugs to suppress increased prolactin synthesis (if the amount of the hormone is excessive).
The goal of such therapy is to stimulate ovulation so that healthy eggs begin to exit into the fallopian tube again.
Important! You should not take hormonal pills on the advice of friends or on your own. Treatment is the prerogative of the doctor.
Such a complex condition can be cured in 2-3 months with an integrated approach. However, pills alone will not help the matter. It is necessary to follow a diet low in animal fats. The diet should be sufficiently fortified. 80% of proper nutrition consists of products of plant origin. There is no talk of any alcohol at all.
Causes of the condition
The following factors can provoke the development of an increased number of follicles:
- Puberty period.
- Lack of a regular menstrual cycle.
- Severe stress, nervous tension.
- Taking oral contraceptives.
- Breastfeeding period.
- Sudden weight fluctuations.
- Polycystic ovary syndrome.
These conditions provoke an insufficient amount of luteinizing hormone (LH), and FSH begins to enhance the stimulation of follicle maturation. It is worth noting that multifollicular ovaries are not a separate disease, but only one of the symptoms that may indicate a number of pathologies.
Folk remedies
Treatment with folk remedies for multifollicular gonads can be a good help in therapy. Doctors identify the most effective herbs:
- sage.
Sage for multifollicular ovaries is considered an effective phytotherapeutic agent. Take it as follows: take 1 teaspoon of raw material, brew in a glass of water. Let it brew for 15 minutes. Drink in two doses during the day. Course - 7-12 days.
- hog uterus.
Borovaya uterus is a universal remedy for the treatment of gynecological pathologies. It is worth taking one and a half teaspoons of crushed raw materials. Pour a glass of boiling water. Leave for 10 minutes. Take three teaspoons per day. The course activities are cyclical. Dosage regimen: take the drug for 2 weeks over a month, then take a break for the remaining 14 days. At the end of the break, take the boron uterus again. Continue this way for 6 months.
In combination, these methods are sufficient for treatment. Systematic therapy will also help answer the question: how to get pregnant with multifollicular ovaries?
Treatment with folk remedies is by no means a panacea. Moreover, self-administration is strictly contraindicated. Sage and hogweed affect reproductive function and hormonal levels, so you should consult your doctor before use.
Multifollicular changes are a variant of the physiological norm in most cases. However, such a condition is not always harmless. The main complications are menstrual irregularities and infertility. As soon as ovulation stops, you should immediately consult a doctor. This is the most correct solution.
Is it possible to get pregnant with multifollicular ovaries?
Multifollicular ovaries and pregnancy – is this compatible? This question interests all women who have been given this diagnosis. It should be noted that multifollicular changes in the ovaries are not considered a pathological abnormality and in itself cannot be a cause of infertility. This condition does not in any way affect a woman’s ability to become pregnant, however, inhibition of the conception process is possible, since due to this pathology the menstrual cycle is disrupted, making it difficult to determine the period of ovulation. Moreover, in some cases, menstruation may be absent for several months, which is due to the fact that none of the follicles, due to multifollicularity, reaches the dominant size, which is why ovulation simply does not occur.
Considering the above, the combination of multifollicular ovaries and pregnancy is quite possible, but requires more careful attention and, if necessary, additional research.
Thus, the answer to the question “is it possible to get pregnant with multifollicular ovaries?” will always be positive.