The occurrence of cystitis after ovulation
Changes in a woman’s body during and after ovulation affect all organs and systems. The bladder is also no exception; inflammatory processes often occur in it. The favorable conditions created for the proliferation of pathogenic flora and its further spread put the entire female genitourinary tract at risk.
Bladder inflammation is considered one of the most common “female” diseases. According to statistics, men are five times less likely to be susceptible to this pathology. In part, this can be “blamed” on the physiology of the weaker sex and the instability of hormonal levels. And cystitis after ovulation is common.
Factors that depress the female body weaken the immune defense of the urinary system, creating favorable conditions for the spread of infection from the external genitalia up the urethra into the bladder. A woman's wide and short channel allows bacteria to move more quickly than a man's. Hormonal fluctuations in ovulatory phases increase the likelihood of inflammation in the pelvis.
Causes of cystitis
When the bladder is affected by pathogenic bacteria, this leads to decreased immunity. One of the most common causes of cystitis is unprotected sex. Sex without the use of contraceptives often leads to urethritis. This pathology occurs due to excessive mobility of the vaginal mucosa.
Factors provoking this disease:
- Hypothermia. It not only weakens local defenses, but also contributes to a decrease in the body's immune function.
- Mechanical injury to the mucous membrane. This can be caused by active sexual intercourse or a diagnostic procedure. Tissue damage facilitates infection of the bladder by pathogenic microorganisms.
- Frequent change of sexual partners. This leads to ureaplasma infection entering the mucous membrane. When foreign flora enters the urethra, there is a risk of an inflammatory process.
- Hormonal disbalance.
- Ovulation. During this period, the number of leukocytes in a woman’s blood increases and the basal temperature rises.
Ovulation in the female body
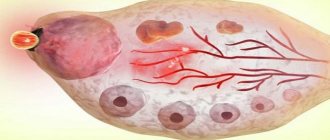
Every month, ovulation divides the menstrual cycle into two parts: the first and second phase. In the first, the follicle matures, which is why it is called follicular. At the beginning, the uterus enlarges, squeezing surrounding tissues and organs, and secretion formation increases. At the end of this period, an egg appears, ready to be fertilized by a sperm. The first day of this phase begins with the arrival of menstruation and lasts about 11-13 days.
In the second phase, luteal, maturation of the corpus luteum is observed, which is formed at the site of release of the egg after ovulation. Progesterone production increases and a woman’s metabolic processes slow down. On average, this period of existence of the corpus luteum takes 13-15 days, at the end of which menstruation occurs. The cycle begins again.
The influence of the process on inflammation in the bladder
A woman’s hormonal background very often predisposes her to the appearance of cystitis both before and after ovulation. Physiological features in this case make the microflora of the genital organs more vulnerable, allowing pathogenic bacteria to penetrate the uterus and bladder. This process is especially pronounced after menstruation.
When a woman's egg is fertilized, hormonal changes intensify. The uterus begins to rapidly enlarge, the bladder is compressed, blood circulation in the pelvis accelerates, and the immunity of the genital organs decreases. These factors contribute to the appearance of interstitial cystitis, a non-infectious inflammation of the bladder, most often characteristic of ovulation. At the same time, the increased level of progesterone weakens the tone of the bladder, urine stagnates, leading to the proliferation of opportunistic microbes.
During the transition from the follicular phase to the luteal phase, fertilization does not always occur, but in both cases an increase in basal body temperature is observed. If this factor is of great importance during menstruation, there is reason to assume the development of cystitis. In addition, during “critical days” women note frequent urination. This is due to the increase in the size of the uterus, which puts pressure on the bladder. However, just such a symptom is not a sign of inflammation in the pelvis.
During
If pathological bacteria penetrate the urethral canal and reach the bladder during the release of a mature egg from the ovary, the patient may complain of pain in the lower abdomen. When symptoms persist for more than 3 days or a woman’s condition worsens (body temperature rises, signs of intoxication appear, etc.), this may indicate that the inflammatory process has spread to the reproductive organs.
When symptoms persist for more than 3 days, this may indicate that the inflammatory process has spread to the reproductive organs.
During ovulation, the uterus enlarges. It puts pressure on the bladder, which causes frequent urination.
Reasons for the development of cystitis in women
Negative deviations can occur in the female urinary system during the period of change of ovulatory phases, when protective functions are suppressed by hormones. It is this factor that is decisive in the development of cystitis.
Before ovulation
Before ovulation occurs, an inflammatory reaction can often be observed in the mucous membrane of the bladder. Often this indicates a chronic form of untreated cystitis, and not about the characteristics of female physiology. In this case, the pathology is called preovulatory.
The provoking factor of the disease is the hormone estrogen, which, despite all the positive effects on the protection of the woman’s body, “gets out of control.” Epithelial renewal is carried out with a slow “utilization” of dead cells, as a result of which they begin to accumulate in the bladder, and this leads to inflammation.
The safety of ovulation is created, oddly enough, by weakening the body’s immune forces to reduce the aggressiveness of phagocytes. But as a result, inflammation of the bladder often occurs.
At ovulatory peak
The process of release of an egg from the follicle occurs at the peak of the ovulatory phase. Its symptoms are similar to those of cystitis. At the same time, hormonal changes are observed, progesterone is produced, and the uterus becomes soft, its immune defense and the level of leukocytes in the mucus decrease. This serves as a favorable environment for the movement of bacteria, viruses, and fungi through the urethral canal into the bladder.
During critical days
When menstruation occurs, pathogenic microbes can easily penetrate both the bladder and the uterine cavity and fallopian tubes. The blood transports them along the ascending path, without encountering obstacles in the microflora of the genital organs. If sanitary pads are used for a long time and are rarely changed, the infection develops faster than in the non-menstrual period.
The main principles of cystitis prevention include adherence to personal hygiene standards, frequent changes of underwear and refusal to wear tight clothing, especially trousers and tight panties such as thongs.
Disease prevention
If you do not receive treatment and do not use preventive methods, you can encounter a connection between ovulation and cystitis every cycle. To avoid this it is advisable to:
- eradicate infection in a timely manner, especially from the intestines and genitourinary system;
- take medications that strengthen the immune system;
- do not neglect personal hygiene.
To prevent intestinal bacteria from getting into the vagina when washing, you need to make proper cleansing movements with your hand - from front to back, and not vice versa.
Prevention of bladder infections includes an active lifestyle, the habit of drinking plenty of clean, fresh water and little alcohol. You cannot swim in unheated water in polluted reservoirs, or sit in cold water. It is also important not to endure the desire to go to the toilet. This weakens the tone of the bladder, and pathogenic bacteria accumulate in the urethra.
If symptoms of inflammation appear, you should immediately contact a urologist. Only a doctor can identify its cause and prescribe the correct treatment.
Most often, cystitis is observed in women (they get sick eight to ten times more often than men). There are a number of reasons for this. Firstly, the structural features of the genitourinary system (the female urethra is wider and shorter than the male one), and secondly, hormonal changes during the menstrual cycle. I would like to especially emphasize that one of the common causes of cystitis is ovulation. Let's try to figure it all out.
With ovulation, the chance of developing cystitis increases
How does ovulation affect the development of inflammation in the bladder?
As already mentioned, in women, cystitis can very often occur after or during ovulation. The reasons for this lie in the following: the immune system from pathogens is weakened, which primarily promotes the activation of opportunistic flora (vagina and intestines). The female body is also weakened after menstruation, which is another reason for the development of disease in the bladder.
The fact is that if ovulation ends with fertilization, then hormonal changes begin in the woman’s body, the uterus enlarges and begins to put pressure on the bladder, the body’s overall immune defense decreases, and the blood supply to the genital organs increases. All this provokes interstitial cystitis. In addition, an increase in progesterone leads to a decrease in bladder tone, as well as stagnation of urine, after which rapid growth and proliferation of pathogenic microbes occurs.
If fertilization does not occur after ovulation, then the monthly cycle moves into the next phase. During this period, the basal temperature in the female body is increased. If this symptom is also detected during menstruation, it may be a sign of cystitis. It is known that frequent urination may occur during menstruation. More often this is due to swelling of the internal genital organs, which causes compression of the bladder. If, in addition to this symptom, a woman no longer has other pathological manifestations, then this is not cystitis.
Cystitis is often caused by bacteria that enter the body when the immune system is weakened.
As practice has shown, the disease most often occurs in the autumn-spring period, since it is at this time that it is easiest to become hypothermic. The etiological factors of cystitis in most cases are pathogenic bacteria, less often viruses and fungi. The causative agent may be a sexually transmitted infection (gonococci, microplasma, chlamydia, etc.). Conditionally pathogenic flora (for example, some representatives of strepto- or staphylococcal infections) cause the development of inflammation in the bladder only when immunity is reduced.
Features of inflammation in the bladder, which is associated with hormonal changes
It should be noted that cystitis during or after the ovulation process has its own characteristics. Since at first an inflammatory process of a non-infectious nature develops, only irritation of the mucous layer of the bladder is observed. Further, due to the structural features of the female urethra, infection quickly occurs (infectious cystitis occurs). In this case, infection occurs when pathogenic microorganisms enter the urethra (from the surface of the skin of dirty hands or external genitalia).
I would like to emphasize that ovulation may be accompanied by short-term pain in the projection of the right or left ovary. This phenomenon is considered natural, physiological, if observed within one to two days. If the pain is severe, cutting, and lasting, then this may be a manifestation of inflammatory changes in the bladder (that is, this is how cystitis manifests itself).
Ovulation is characterized by temporary pain, but if it does not go away, cystitis may develop.
Also, pain during the ovulation process, localized in the lower abdomen, can occur with chronic gynecological diseases. In this case, the pain is often cramping and can intensify after overwork, stressful situations, hypothermia, or errors in diet. As a rule, in this case, vaginal discharge is also observed, and women often cannot become pregnant for a long time.
Thus, if ovulation is accompanied by severe pain, headaches, painful urination, shortness of breath and other symptoms, it is necessary to urgently consult a specialist.
Moreover, no matter what causes the appearance of pain in the lower abdomen after the ovulation process, you must be very attentive to your body, promptly seek medical help in order to take the necessary measures in time and prevent the occurrence of dangerous complications.
It should be noted that experts recommend that all women after thirty years of age undergo a detailed examination every year, while visiting a gynecologist twice a year.
Clinical manifestations of cystitis
All manifestations of this disease in women are very pronounced, so it is quite difficult to confuse it with another pathological process. The very first manifestation of inflammatory changes in the bladder is frequent urination, often painful (during or after urination). In this case, the pathological process may be accompanied by an unpleasant burning sensation. Pain may appear along the urinary tract.
With cystitis, frequent and persistent pain appears below the abdomen
Women are also worried about constant aching, sometimes nagging pain in the lower lumbar region and in the suprapubic region (this area is the projection of the bladder), general malaise, and headaches. Cystitis can cause a rise in temperature in patients (up to low-grade or febrile levels).
New acute cystitis or an aggravated chronic process as a result of fluctuations in female hormones has some features. As a rule, it is very painful and leads to menstrual irregularities, often causing delayed menstruation in women.
It should be said that urine visually changes. It becomes cloudy, dark yellow, and impurities are often visible - clots, flakes, etc.
As for the results of a urine test during cystitis, naturally, pathological changes will be noted in it. There is leukocytosis (increased content of white blood cells), a high content of mucus, and may also contain bacteria, less often red blood cells, protein (usually in small quantities). The amount of bacteria in the urine directly reflects the severity of the pathological process. It should be said that if the urine is sterile due to inflammatory changes in the mucous membrane of the bladder, this is the basis for a detailed examination of the woman for the presence of tuberculosis.
The main thing is not to miss the onset of inflammatory changes in the bladder. At the first symptoms of inflammation, you should contact a urologist so that the doctor can prescribe the appropriate tests and ultrasound examination of the genitourinary system. Only timely and adequate treatment will help cope with this female illness.
The causes and extent of the disease can be determined by taking a urine test.
Preventive measures
- To prevent cystitis, it is necessary to strengthen the immune system during and after the ovulation process.
- Timely treatment of infectious processes (genital organs, intestines).
- Maintain personal hygiene, especially during menstruation (it is important to note that when washing, it is necessary to make movements in the front-to-back direction, in this case there is minimal possibility of introducing an infection from the anal area to the urethra and vagina).
To summarize, I would like to especially emphasize the danger of cystitis, which consists in very difficult treatment, and most importantly, that the pathological process is almost impossible to cure completely. In women, the provoking factor is always either ovulation or menopause.
The next video will talk about ovulation:
A large number of women experience bladder inflammation. This disease occurs against the background of various negative factors. In some cases, cystitis may develop after ovulation. This period in the body of women is characterized by the fact that it becomes more vulnerable to pathologies of infectious etiology.
Increased urination: is it always cystitis?
Frequent urination is not always a sign of bladder inflammation. In the absence of pain, itching and burning in the urethra, increased urination cannot indicate cystitis after or before ovulation. The uterus, which cyclically changes in size, compresses the excretory organ, accordingly leading to its frequent emptying.
However, cystitis is not determined by this symptom alone. A woman’s “biological clock” contributes to uncomfortable symptoms such as frequent urination, which do not require medical intervention. The true illness is complicated by other symptoms, quite unpleasant, which are not easy to tolerate. With inflammation, the structure of urine changes, it becomes cloudy, with visible inclusions, and a pungent odor appears.
Cystitis as a manifestation of pregnancy
Women are characterized by physiological conditions that can be confused with pregnancy. Their symptoms include not only delayed menstruation, but also an increased urge to urinate. However, the cyclicity of ovulatory and menstrual periods is the first thing every girl should monitor. If monitoring is not done in a timely manner, false assumptions may arise during pregnancy.
When an egg is fertilized, the body begins to rebuild itself to preserve the fetus, signaling, for example, by frequent urges to go to the toilet. The uterus does not change its size much during this period, so the increase in the number of urinations is associated with other processes. At the beginning of the first trimester, the volume of circulating blood increases, which in turn increases the load on the excretory system.
After
In the second period of the cycle, cystitis may be indicated by: increased body temperature, delayed menstruation or heavy bleeding, unhealthy vaginal discharge. In addition, the color and smell of urine change: it becomes cloudy with the presence of impurities in the form of clots and flakes, acquires a dark yellow color, and has a strong and unpleasant smell.
Diagnosis and treatment of pathology
If inflammatory processes in the bladder are suspected, first of all, specialists determine the composition of urine and blood. After detecting a large number of leukocytes in these fluids, as well as as a result of collecting a pathological history of the patient, the doctor can assume the occurrence of cystitis. To determine the bacterial pathogen, bacterial culture is prescribed.
An additional measure is ultrasound diagnostics of the pelvic organs and bladder. Ultrasound specialists also examine the patient’s kidneys to rule out pyelonephritis. This procedure is necessary when blood or pus is found in the urine, and the inflammation develops rapidly and acutely. In exceptional cases, cystoscopy is performed - examination of the bladder using an endoscope.
In the treatment of cystitis, medications with the following properties are used primarily:
- antibacterial and antiseptic;
- analgesics and antispasmodics;
- antiviral;
- antifungal;
- immunostimulating.
During the treatment period, a diet is prescribed that excludes salty, spicy, pickled, and alcoholic foods. Products are baked or boiled. The menu includes vegetable soups and stews. The amount of clean water in the diet is increased, fruit drinks, sour berry compotes, and green tea with lemon are added.
Features of treatment
At the first signs of cystitis, a woman should consult a doctor who, after examination, will prescribe the laboratory tests and studies necessary to diagnose the disease. After receiving the results and determining the severity of the inflammatory process, the specialist will select an individual course of treatment.
For the treatment of cystitis during or after ovulation, antibiotics, restorative and anti-inflammatory drugs, and diuretics can be prescribed.
In combination with drug treatment, patients often resort to various folk remedies. To get rid of cystitis, you can use medicinal herbs. There are a large number of recipes for decoctions and infusions based on herbal preparations and medicinal plants. In addition, patients are recommended to take baths, washes, microenemas, etc.
Prevention of cystitis
Certain principles contribute to positive dynamics in the treatment and prevention of the disease:
- eliminate unhealthy foods (carbonated water, spicy foods and canned food);
- observe personal hygiene standards, including a daily intimate shower and a change of underwear;
- follow the ban on sexual activity during the treatment of cystitis;
- limit contact with cold surfaces and bodies of water;
- follow medical prescriptions throughout the entire therapeutic course;
- increase your drinking rate;
- maintain bed rest if your doctor recommends it;
- Treat intestinal infections, as well as gynecological ones, such as thrush, in a timely manner.
When excluding bacterial and viral pathogens, experts suggest ovulation as the culprit for the symptoms of cystitis. To treat this condition, gentle herbal-based medications are prescribed. Herbal medicine and other folk recipes are considered an auxiliary norm. However, it is also necessary to strictly follow the doctor’s recommendations in this case, otherwise cystitis will become chronic.
The female body is more complex than the male body. Sometimes we mistake natural physiological processes, such as ovulation, as acquired cystitis as a result of infection with pathogenic bacteria. Visit a urologist in a timely manner if painful symptoms appear, since the true causes of bladder inflammation are determined only in laboratory conditions.
Treatment
If symptoms of cystitis occur, you should seek help from a qualified specialist. First of all, you need to be examined by a urologist. It would also be a good idea to visit a gynecologist.
Treatment of cystitis involves systematic use of medications. Only a doctor should prescribe them. Typically, the symptoms of this disease are controlled with broad-spectrum antibiotics. The recommended course of treatment with such agents is 4–6 days. The urologist will prescribe Norfloxacin or Ciprofloxacin to the woman.
If there are first signs of recovery, it is not recommended to stop taking antibiotics, as this may provoke a recurrence of signs of bladder inflammation. In this case, the disease can develop into a chronic form.
If the inflammatory process began after ovulation, the urologist will prescribe herbal medicines to the patient. Treatment with herbal medications lasts longer.
Traditional methods of treating this disease include taking decoctions made from:
- from bearberry leaf;
- lingonberries;
- juniper;
- millennium;
- barberry;
- raspberries
Before treating cystitis using traditional methods, it is recommended to consult a doctor - a urologist or gynecologist.
Dealing with cystitis is not easy. It is much easier to prevent its occurrence. To do this, it is recommended to avoid hypothermia and promptly treat inflammatory diseases.
Cystitis is considered an unpleasant disease that can occur not only at the stage of ovulation. A woman can also experience bladder inflammation during menstruation. Therefore, we recommend that you read more detailed information on this topic.
Features of the development of cystitis after ovulation
Inflammation of the bladder walls (cystitis) is rightfully considered a common disease among women (men get sick five times less often). And the reason for this is not only the anatomical and physiological characteristics of the urinary system, which facilitates the migration of pathogens into the bladder, but also many purely female, vulnerable factors that negatively affect the immune system.
One of them is ovulation. In urological and gynecological practice, cystitis after ovulation, before it, or in the middle of the ovulatory phase is not uncommon. To understand the mechanism of development of the disease, let us briefly consider the nature of ovulation as such and its relationship with cystitis.
Preventive actions
To reduce the likelihood of pathogenic microflora entering the urethra, a woman needs to wash herself daily. The choice of detergent must be taken responsibly. Some of the substances can cause an allergic reaction, against which cystitis can develop.
CYSTITIS honeymoon
9 reasons for menstrual irregularities. Signs of delay.
What happens to the body during the menstrual cycle
Treatment of cystitis in women in 1 day - without pills. ATTENTION! - read the contraindications!
A woman must promptly treat all infectious processes that occur in her body.
The key to good health is a strong immune system. In order for the body to be resistant to pathogenic microflora, it is necessary to try in every possible way to strengthen the natural protective function of the body.
Attention must be paid to the diet. Spicy and fried foods, pickles, smoking and alcohol are foods that contribute to the development of the disease.
Preference should be given to boiled food, fermented milk products, vegetables, fruits and natural juices.
In the chronic form of cystitis, during the period when ovulation begins, a woman is advised to refrain from prolonged sexual intercourse. Rough and unprotected sex against a background of reduced immunity is another reason for the development of the disease.
Women turn to a gynecologist or urologist with complaints of pain during urination 10 times more often than men. This is due to the structural features of the body and processes characteristic exclusively of the female body. One of them is ovulation.
Ovulation and cystitis: what is the relationship?
The relationship between the development of inflammatory reactions in the bladder organ and the process of ovulation can be traced in any woman who has reached reproductive age with established regulative (menstrual) phases. Like the regula, a woman’s body experiences monthly periods of ovulation—the maturation of an egg awaiting fertilization.
The ovulatory period is closely related to the menstrual cycle and divides it into certain phases - the follicular, pre-regular, ovulation phase itself and the luteal phase, starting from the second half of the menstrual cycle.
Follicular phase
This is the preparatory period of the ovulation process, characterized by increased pituitary hormonal secretion, stimulating the production of estrogen and the maturation of eggs. The maturation of the germ cell takes place in the liquid medium of the graafian sacs (follicle vesicles).
Follicle-stimulating hormonal secretion ensures the achievement of maturity of the 1st and 2nd follicles and the secretion of estrogen. At the beginning of the regulation, the estrogen level is insignificant. Its increase occurs in parallel with follicular maturation.
During the process of follicular development, one or several vesicles in which the egg matures lead in size over the others, and are the first to reach the preovular state.
The secretion of estrogen constantly increases, preparing the zygote (fertilized cell) “comfortable” conditions for development and growth (saturates the mucous cavity of the uterus with blood and nutrients), controls mucous secretion, providing favorable conditions for the advancement and survival of sperm.
Dependence of cystitis on ovulation
The menstrual cycle affects the functioning of all body systems. This is due to the fact that when the egg matures, the hormonal levels change several times.
The main substances produced by the female reproductive system are estrogen and progesterone.
Ovulation is the maturation of an egg. When the egg matures, it leaves the follicle and begins to move towards the uterine cavity. Thanks to hormonal changes, optimal conditions are created for this.
Ovulation occurs in the middle of the menstrual cycle. You can determine the exact date of egg maturation by measuring basal temperature.
Each woman has a different menstrual cycle, and ovulation occurs individually for each woman.
During ovulation, the most important changes for the development of cystitis occur, which include:
- Increased blood supply to the uterus. Increased blood flow in the uterine area leads to ischemia of nearby organs. As a result of insufficient blood supply, local immunity in the bladder decreases. This situation is fraught with the fact that even a small amount of bacteria leads to the development of the acute phase of the disease.
- Enlargement of the uterus. Under the influence of hormones, the functional layer of endometrial cells increases several times, and the uterus enlarges. This leads to compression of the remaining pelvic organs. This phenomenon aggravates the ischemic condition in them.
- Local decrease in body temperature. With the onset of ovulation, there is a decrease in basal temperature. This is so that the sperm reaches the egg and does not die, since low temperatures are comfortable for it.
Such processes contribute to the development of the inflammatory process. Regardless of whether cystitis depends on ovulation, full treatment is carried out.
Development of cystitis in the preovular period
It should immediately be noted that the development of inflammatory processes in the mucous lining of the bladder is not a pattern, nor is it a primary process. Rather, the manifestation of cystitis before ovulation is due to an exacerbation of its chronic course.
Many factors can provoke preovular cystitis. The main one is the rapid increase in estrogen secretion. It would seem that estrogens are a priori protectors of the female body, but in this case, their “good” effect, aimed at rapid cellular renewal and destruction of pathogens in the bladder reservoir, is disrupted by the most unexpected influence of various factors.
As a result, in the follicular phase (at the beginning of regulation) in the cavity of the bladder there is an accumulation of dead epithelium, which contributes to incomplete emptying with signs of residual urine in the reservoir cavity of the bladder - an excellent soil for the activation of pathogenic microorganisms and the development of inflammatory processes in the tissues of the bladder.
An excellent breeding ground for infection is blood. With its abundant secretion at the beginning of regulation, any violation of hygiene leads to additional formation of a source of infection.
Promotes the activation of the chronic clinic of infectious-inflammatory lesions of the MP - weak immune defense. This is a physiological factor aimed at reducing the aggression of phagocytes (cleaner cells), which ensures the safety of the ovulatory process.
What to do at the first symptoms of cystitis?
The first step in treating cystitis is to eliminate the causes of the disease. You should not undertake self-treatment. Adequate antibacterial therapy must be selected by a doctor. Medicines are prescribed with high activity against the causative agent of the disease and creating high concentrations in the urine and tissues. In this case, preference is given to drugs that are taken once a day.
The first signs of cystitis can be eliminated not only by taking antibiotics, but also by following the following recommendations:
- exclusion of salty, fried, spicy foods from the diet;
- refusal of alcohol, tea, coffee;
- drink more water (1.5-2 liters per day);
- use a natural diuretic: cranberry, parsley, watermelon.
An important point is to prevent relapses. It is recommended to urinate every 3-4 hours, even if there is no feeling of bladder fullness. There must be urination after sexual intercourse, especially open sex. But the main preventive measures are maintaining personal hygiene.
Manifestation of the disease at the stage of ovulation
The release of a mature cell from the Graafian vesicle, in anticipation of becoming a zygote - a diploid cell (fertilized), causes an active hormonal surge, followed by a gradual change in hormonal phases (estrogen and progesterone). In addition, the ovulation process is accompanied by various accompanying symptoms that can provoke cystitis during ovulation. They are due to:
- An increase in body temperature at rest, measured rectally (basal temperature), caused by increased blood circulation in the uterine walls and due to the expansion of venous trunks and vessels.
- Increased secretion of secretions, creating a breeding ground for pathogens and creating increased humidity, causing hypothermia of the MP.
- The influence of antihistamine enzymes and hormones responsible for immune regulation processes, which reduce the physiological process of phagocytosis at this stage. The protective mechanism is laid down by nature to protect the fertilized zygote from being rejected by the body as a foreign body.
- Swelling of the body of the uterus and swelling of its walls, which leads to displacement of adjacent tissues and organs and, as a result, disruption of urinary outflow from the bladder cavity.
During the period of ovulation, exacerbations of other chronic foci of infection are possible and inflammatory processes in the bladder tissues can manifest themselves as a consequence of migrating infections. It is difficult to distinguish the signs of cystitis during this period. Soreness, fever and frequent micturition (urination) are characteristic of these two conditions.
The only difference by which cystitis can be suspected is the duration of symptoms. The ovulation process lasts no more than a day and a half, and if the pathological symptoms have a long course, then it’s time to start treatment.
How does the disease manifest itself?
Cystitis in women is easily determined by differential diagnosis, as characteristic complaints appear that are difficult to confuse with anything.
Provoking factors, for example, hypothermia, lead to the sudden appearance of the following picture:
- frequent and painful urination up to 150 times a day;
- pain in the perineum and in the projection area of the bladder;
- bleeding at the end of emptying associated with damage to the bladder neck;
- the urine is cloudy due to the presence of red blood cells, white blood cells and bacteria.
The stronger the inflammation, the more often the urge to urinate and the more severe the pain. Painful impulses contract the muscular lining of the bladder, and the urge to urinate occurs. In acute uncomplicated cystitis, there is rarely an increase in temperature.
If the temperature rises, pain is felt in the lumbar region - these are signs of the development of acute pyelonephritis.
Chronic cystitis, unlike acute cystitis, can manifest itself in different ways - slight discomfort and acute sudden pain with frequent urination (pollakiuria). The frequency of relapses and remissions may vary and depends on the presence of provoking factors.
It is important not to let the disease get worse!
Inflammatory lesions of the bladder after ovulation
It cannot be said that after the ovulatory period, inflammatory processes in the bladder tissues must necessarily develop. As with any period of this process, the risk of developing the disease is determined by a combination of circumstances and a combination of provocative factors.
Hormonal imbalance affects the pathogenic flora of the urinary system, which provokes an exacerbation of chronic infectious pathologies.
Increased secretion of progesterone in the final (luteal) phase of ovulation leads to disruption of the tone of the detrusor (muscle tissue) of the bladder, which disrupts the processes of urethral outflow and leads to stagnation of urine, opening the way to primary infection.
Increases the risk of developing the disease:
- weakened immune system;
- the presence of vaginal dysbiosis and sexually transmitted infections;
- neglect of the rules of hygiene of the intimate area;
- allergic predisposition to medications and hygiene products;
- prolonged exposure to cold.
In any phase of ovulation, cystitis can be distinguished from ovulatory syndrome by changes in urine - cloudy, dark in color, with admixtures of mucus, flakes or bloody clots.
Whatever processes contribute to the development of inflammatory reactions in the bladder reservoir after ovulation, therapy must be complete and timely. Without professional diagnostics to identify the cause, self-medication will not bring results, but will only aggravate the process, which will lead to a chronic clinical course with frequent relapses.
What is cystitis
There are several forms of the disease:
- Microbiological: the disease is caused by a specific pathogen, often of bacterial origin;
- Neurological: more often typical for children of senior preschool and primary school age, as well as for people with an unstable psyche;
- Dysplastic: occurs as a result of abnormal structure of the urethra or anomalies of other urinary organs, which either interfere with the natural outflow of urine or create excellent conditions for the penetration of pathogenic bacteria;
- Caused by a third-party infectious focus, by transferring infection through the bloodstream: periodontal disease, joint diseases, inflammation of the gastrointestinal tract;
- Postoperative: inflammation develops as a result of stagnation of fluid (including urine) in the body;
- Hormonal: develops as a result of hormonal changes in the body.
Causes of cystitis before, during and after ovulation
Cystitis is an inflammatory process of the mucous membrane of the bladder. It most often occurs in women and is caused by hypothermia.
Symptoms include frequent urination and pain during and after it. The cause is bacteria that enter the urethra from dirty hands and external genitalia. Another cause of the disease is viruses and pathogenic fungi.
Symptoms of cystitis include frequent urination and pain during and after it.
Ovulation and cystitis
Ovulation is the phase of the menstrual cycle in which a ready-mature egg is released into the uterine cavity for subsequent fertilization. During this period, there is an active surge in the entire hormonal system of the body, as well as a gradual change in the estrogen and progesterone phases.
In addition, ovulation is accompanied by a number of concomitant symptoms, which contribute to the development of bladder inflammation during this period. These include:
- An increase in basal temperature, which is caused by increased blood flow to the uterus, as well as dilation of blood vessels and most ducts of the body;
- An increased amount of secretions, which a) create excellent microflora for the life of various pathogens (especially E. coli and fungi of the genus Candida) and b) create a feeling of increased “phlegm”, which in turn can cause hypothermia of the bladder.
- Physiological decrease in immunity - at this stage, antihistamine enzymes and hormones responsible for the regulation of immunity are actively activated. This mechanism is provided by nature so that the egg, in the event of fertilization, is not rejected by the body;
- An increase in the size of the uterus, which leads to slight compression of surrounding organs and tissues and, as a result, disruption of the outflow of urine from the bladder;
Ovulation contributes to the exacerbation of other chronic infectious foci, and cystitis can be a consequence of a “migratory infection.”
What is ovulation
Ovulation accompanies a woman from the first critical days until the onset of menopause. Once a month, approximately in the middle of the menstrual cycle, an egg that is ripe for conception leaves the ovary. If a sperm manages to fertilize it within 24 hours, pregnancy occurs. Otherwise, it will come out along with bloody discharge.
If you are planning a child, or, conversely, avoiding “dangerous” days, you should know when ovulation occurs. Usually it occurs on the 14th day, but it is more effective to calculate this moment, starting from the individual cycle length.
Hormonal surges and decreased immunity during this period can lead to the development of diseases of the genitourinary system. Most often cystitis or thrush.
Features of the manifestation of cystitis during ovulation
The main feature of the development of bladder inflammation in the ovulatory period is the fact that it is very difficult to diagnose the disease itself, since it is often erased in symptoms characteristic of ovulation:
- Pain during ovulation can be either from the ovaries or downwards;
- There is a slight increase in basal temperature, which can either be present with inflammation or be observed with cystitis;
- Due to the fact that the bladder is slightly compressed by the enlarged uterus, there may be frequent urination.
A distinctive symptom that allows you to separate inflammation from ovulatory manifestations will be the presence of cutting pain when urinating. Time will also be an important factor - if the pain lasts more than 2 days, it is important to begin the treatment process, because the average duration of ovulation does not exceed 36 hours.
Is cystitis associated with ovulation?
Ovulation is the release of an egg from the ovaries. During this period, the likelihood of bladder infection increases. The end of the menstrual cycle contributes to the weakening of the female body and, as a result, the development of pathology.
During ovulation, pathogenic microorganisms quickly penetrate into the female genital organs. This leads to cystitis and other diseases of the genitourinary system.
Since the immune system is weakened during the period of hormonal changes, pathogenic bacteria that provoke the inflammatory process exist in a comfortable environment.
Hormonal changes during this period are associated with the movement of the egg through the fallopian tubes. It is very important to observe the rules of personal hygiene during ovulation, since otherwise the risk of bladder inflammation increases several times.
With this disease, an increased number of leukocytes is present in the vaginal discharge.
What symptomatic complex is observed:
Painful sensations: with cystitis during the ovulatory period, they can easily be confused with radiating pain of the uterus itself, as well as reflex responses from other organs, but nevertheless, characteristic cutting sensations can be identified that go to the urethra when the bladder is filled;
Temperature: it rarely rises above 37.5°C, even during the period of hormonal transition characteristic of ovulation;
Frequent urination is the most relevant sign for cystitis. Occurs as a result of irritation of the mucous membrane of the bladder;
Weakness, weakness, fatigue are phenomena characteristic of both hormonal changes and the onset of the disease.
From the analysis side:
- an increase in leukocytes and ESR will be recorded in the blood, which will indicate an inflammatory process in the body;
- protein may appear in the urine, and its character will also change (the urine becomes cloudy, not transparent, the color may have a greenish tint due to the release of a large number of destroyed leukocytes, there may be white inclusions).
Treatment of cystitis during the period of ovulation comes down to the same methods as the treatment of a disease that appears during the normal period.
If cystitis began immediately after ovulation, you can limit yourself to treatment with phytocomplexes and traditional methods.
Phytocomplexes: preparations based on natural components aimed at alleviating symptoms and strengthening the urinary system: canephron, phytolysin, cystone, etc.
Folk remedies: cranberry juice, decoction of bear ears, barberry, yarrow, knotweed, calendula tincture.
Increased heat to the inflamed area (if there are no other concomitant diseases); Drink plenty of fluids.
If the disease does not go away in the next 2 days, then this indicates the addition of an infectious process and requires consultation with a urologist and the prescription of stronger therapy. In particular, you should be wary of the presence of blood in the urine; this may indicate:
- On the involvement of the kidneys in the inflammatory process;
- About injury to the walls of the bladder (if the inflammatory process provoked the release of sand or stone);
- About rupture of small vessels of the bladder wall;
- About the presence of oncological changes in the bladder or ureters.
However, before you become alarmed by seeing red-colored urine, you should first analyze all the foods you have previously eaten. It should be remembered that foods such as beets and some medications and food coloring can turn urine red.
When an inflammatory process is diagnosed, in addition to the classical methods of treating cystitis at home, specialized antibiotics are prescribed for a period of 3 to 7 days (ciprofloxacin, ciprova, monural uromycin, norfloxacin, etc.), and in some cases physiotherapy.
Clinical picture of the disease
Women who have heard about frequent urination as a sign of inflammation can “diagnose” the disease themselves. But this behavior of the body during critical days may be a consequence of slight swelling of the organs and compression of the bladder. The following symptoms indicate the presence of inflammation:
- burning in the groin;
- pain during or at the end of urination;
- cloudy urine with an unusual odor;
- urinating more often than usual.
The clinical picture may be accompanied by general weakness and fever. Sharp pain in the bladder is reflected by a nagging pain in the lower back or lower abdomen. But even if all the signs are present, you cannot self-medicate. For example, women advise each other to simply lie down with a warm heating pad. It is necessary to consult a urologist for diagnosis.
Prevention of cystitis
Preventive measures aimed at preventing this inflammation come down to:
- Strengthening immunity;
- Treatment of concomitant diseases;
- Prevention of hypothermia;
- Compliance with the necessary diet, excluding excessive consumption of fast food, salt, irritating seasonings, and in some cases oxalic acid products;
- Compliance with the rules of personal intimate hygiene.
Sources:
https://nefrox.ru/symp/cistit-posle-ovulyacii.html https://mycistit.ru/vid/posle-ovulyacii https://ovulyacia.ru/problemy/cistit-pri-ovuljacii