Adhesions after hysterectomy
Hysterectomy or removal of the uterus is a common operation in modern gynecology.
Surgery to remove or amputate the uterus is often performed in women after forty years of age. This is due to the fact that in patients of reproductive age, hysterectomy is performed only for serious indications. Hysterectomy, which involves amputation or removal of the uterus, is performed in the following clinical cases:
- uterine rupture during delivery;
- intensive growth of benign tumors in women after menopause;
- malignant tumors of both the uterus and appendages, as well as suspicion of an oncological process;
- uterine prolapse in the presence of concomitant pathologies.
Sometimes the uterus is removed in case of extensive injuries in the pelvis and purulent peritonitis, which are characterized by a severe course. The issue of amputation of the uterine body is decided on an individual basis and depends, first of all, on the severity of the pathologies, the presence of other diseases, the age and reproductive plans of the patient.
Hysterectomy can be performed using several techniques.
- The most common is supravaginal removal or amputation.
- Extirpation of the uterine body with appendages involves amputation of both the cervix and both ovaries.
- Total hysterectomy means removal of the uterus along with the appendages, cervix, ovaries, local lymph nodes and affected vaginal tissue. This type of removal is recommended for malignant uterine tumors.
Gynecologists note the following surgical and postoperative complications.
- Inflammation and suppuration of the postoperative suture. In this case, swelling, redness, and suppuration of the wound develops with possible symptoms of dehiscence of postoperative sutures.
- Suture infection after surgery. Symptoms of infection include high fever and soreness. In order to prevent infection, the postoperative suture needs regular treatment.
- Urinary dysfunction. In the early postoperative period, pain often occurs when emptying the bladder.
- Bleeding. This complication can occur both during the surgical and postoperative periods.
- Damage to neighboring organs. When amputating the uterine body, damage to the walls of the bladder and other organs is possible.
- Pulmonary thromboembolism. This dangerous complication can cause blockage of the pulmonary artery with pieces of torn tissue.
- Intestinal paresis. Occurs against the background of damage to the nerve fibers of the pelvis during surgery.
- Peritonitis. This pathology means inflammation that has spread to the abdominal area. If this postoperative complication is not eliminated in time, there is a risk of developing sepsis. In this case, the woman experiences symptoms such as severe pain, loss of consciousness, sallow skin tone, intense sweating, and high fever. Treatment consists of antibiotics and removal of the uterine stump.
Later consequences include the following manifestations.
- Loss of reproductive function. Removal of the uterus makes it impossible to carry a pregnancy.
- Psycho-emotional disorders. Hormonal fluctuations cause an unstable emotional background, a depressed state, and irritability.
- Decreased libido. A woman may notice a lack of sexual desire. Sexual life is characterized by pain and psychological discomfort.
- The appearance of symptoms of early menopause. After amputation of the uterine body, symptoms such as sweating, hot flashes, and bone fragility appear.
- Development of the adhesive process. After any surgical intervention, the appearance of adhesions is considered inevitable.
- Cosmetic defect. Since amputation of the uterus most often occurs through abdominal surgery, a noticeable scar remains.
After removal of the uterus by hysterectomy, postoperative adhesions occur, which can lead to unpleasant symptoms, for example, pain, problems with defecation and urination, displacement of the pelvic organs, and prolapse of the vaginal walls.
Uterine fibroids and pregnancy
Quite often, women of reproductive age have questions regarding the possibility of pregnancy, both with fibroids and after surgery to remove them. Making the right decision regarding the management tactics of a particular patient is a very important step, and it should be based on objective literature data, the capabilities of surgeons and generally accepted standards of examination and treatment.
In this section you can find answers to basic questions related to uterine fibroids and pregnancy, as well as laparoscopy and pregnancy.
Is it possible to plan a pregnancy if you have uterine fibroids?
The answer to this question depends on many factors that need to be taken into account:
1. Localization (location) of the myomatous node.
If the myomatous node is located in the uterine cavity, or in the wall of the uterus in such a way that it deforms the cavity, or in the isthmus (cervix) of the uterus, then in this case pregnancy is physiologically impossible. Roughly speaking, nodes of this arrangement play the role of a spiral, i.e. play a contraceptive role. Sperm simply “settle” on the surface of such nodes, without reaching the fallopian tube. Thus, a “meeting” of an egg with a sperm is impossible. Such nodes must be removed!
If the myomatous nodes are small in size, located in the thickness of the uterine wall (on average up to 3-4 cm) or located outside, i.e. have subserous localization, then in this case there is no deformation of the cavity, and pregnancy can occur under other satisfactory conditions. With such nodes you can plan a pregnancy. In the future, problems associated with pregnancy are possible, however, their frequency according to the literature averages 15-20%.
If there is a node on a thin stalk, during pregnancy there is a high risk of torsion, which will lead to the need for emergency surgery and possible termination of pregnancy. To prepare for pregnancy, such nodes also require preliminary removal!
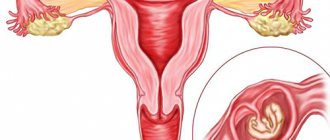
The figure below schematically shows myomatous nodes that do or do not require surgical treatment:
Figure 1. Different localization of myomatous nodes.
2. Tendency of uterine fibroids to rapid growth If, according to ultrasound and observation, uterine fibroids tend to grow rapidly, i.e. increases its size by 1.5-2 times within six months, then in this case it is impossible to plan a pregnancy with uterine fibroids. This is associated with a high risk of fibroid growth during pregnancy, the possibility of malnutrition in the myomatous node, as well as the risk of miscarriage. In this case, surgical treatment is first necessary.
3. Sizes of myomatous nodes In the presence of large uterine fibroids, i.e. If the size of the uterus exceeds 10-12 weeks of pregnancy (and when performing IVF in the presence of uterine fibroids more than 4 cm in diameter), you should not plan a pregnancy either, since there is a high probability of miscarriages and malnutrition during pregnancy (this will require emergency surgery). And the pregnancy itself, i.e. its occurrence is unlikely, since in 60-70% of cases the presence of such fibroids is accompanied by endometrial pathology, which leads to the impossibility of embryo implantation.
According to the literature, it is also known that after removal of myomatous nodes, the probability of miscarriage is significantly lower!!!
What happens to uterine fibroids during pregnancy? Is she growing or not?
It is impossible to predict the “behavior” of uterine fibroids during pregnancy. In all likelihood it is due to genetic predisposition. According to world literature, it is known that 65-75% of myomatous nodes decrease in size by an average of 30%. However, 25-35% of myomatous nodes can grow during pregnancy, and their volume, as a rule, increases by 2 times, i.e. 100%
Laparoscopy or laparotomy? What access should be used to remove myomatous nodes when planning pregnancy?
The question of access to surgical intervention for uterine fibroids is quite complex. Very often, patients ask the question: “Laparoscopy and pregnancy after removal of uterine fibroids - is it possible?”
On the one hand, laparoscopy has a large number of advantages, the main one of which is a significant reduction in the likelihood of the formation of adhesions in the pelvis. In the future, this allows you to maintain the patency of the fallopian tubes, which is one of the important factors during pregnancy. When performing laparotomy, the likelihood of the formation of adhesions is much higher, and their formation is possible not only in the abdominal cavity, but also in the pelvis. In the future, this leads not only to infertility, but possibly also to complications from the gastrointestinal tract (for example, adhesive intestinal obstruction).
On the other hand, it is believed that with large size myomatous nodes, it is not always possible to suture the uterus as needed during laparoscopy. This is due to the peculiarities of laparoscopic technology, a certain angle of the abdominal instruments, and many technical issues. In general, according to world literature, the quality of uterine scar healing depends on:
- on the characteristics of the body (nature of wound healing)
- quality of uterine suturing (scar formation, layered suturing, degree of coagulation of wound edges, correct comparison).
To summarize the above, we can state that the optimal (maximum) size of nodes for laparoscopy for women planning pregnancy are myomatous nodes measuring 5-6 cm. To suture the uterus with such myomatous nodes, the special skill of the surgeon is required. For large nodules, new technologies for suturing the uterus have been developed, which can be used to strengthen the uterine wall, but the risk of uterine rupture along the scar in such cases is always higher.
In the presence of myomatous nodes more than 9-10 cm in diameter, the risk of uterine rupture along the scar exceeds the risk of the formation of adhesions after laparotomy. In this case, it is optimal to refuse gentle access and perform transection taking into account the reproductive wishes of the woman.
Do adhesions form after laparoscopy when removing uterine fibroids? Is it necessary to do a control laparoscopy?
The incidence of adhesions formation during laparoscopy for conservative myomectomy is significantly lower than during transection, i.e. laparotomy. (this is also related to the question “Laparoscopy and Pregnancy”) However, with large size nodes, concomitant adhesions, the presence of endometriosis and inflammation of the uterine appendages, genetic characteristics of the body, in the postoperative period there is a risk of recurrence of the adhesions. According to the literature, the likelihood of the formation of adhesions after laparoscopy for removal of uterine fibroids is higher if the myomatous node is located on the posterior wall of the uterus. The reasons for this phenomenon are currently unclear. Most likely this is due to gravitational factors (blood flow into the retrouterine space) and the anatomical features of the structure of the female genital area.
In the presence of concomitant pathology (endometriosis, chlamydia and gonorrhea in the anamnesis, etc.) in women interested in pregnancy, control laparoscopy is indicated after 6-8 months to assess the condition of the fallopian tubes. The issue of repeat surgery is decided individually each time, taking into account many factors and medical history.
When performing a laparotomy for the removal of large myomatous nodes, due to the high probability of the formation of adhesions, it is optimal to perform a control laparoscopy to restore the patency of the fallopian tubes due to the high risk of their obstruction.
After what period of time can I plan a pregnancy after surgery?
After removal of uterine fibroids by any access (laparotomy, laparoscopy), pregnancy is resolved after 8-12 months, which depends mainly on the size of the removed node. Given its small size (on average 3-4 cm), pregnancy planning is possible after 8 months. These limitations are associated with the healing characteristics of the uterine muscle. On average, only the resorption of sutures is completely completed after 90 days from the date of surgery. Considering the fact that during pregnancy there is a very significant increase in size of the uterus, i.e. its muscle fibers stretch and hypertrophy quite strongly; complete healing of the uterine scar is necessary to plan pregnancy.
Is it always necessary to have a caesarean section after a myomectomy?
Indications for caesarean section are determined individually each time and depend on:
- on the size of the myomatous node that was removed, i.e. uterine scar size
- its previous localization
- the presence of concomitant indications during pregnancy and childbirth (for example, the woman’s age, the presence of gestosis, duration of infertility treatment, etc.)
- Ultrasound examination data of the scar during pregnancy
In general, with the previous removal of uterine fibroids up to 3-4 cm in diameter, the woman’s young age, the absence of complications during pregnancy and childbirth, and the satisfactory condition of the uterine scar according to ultrasound, it is possible to conduct childbirth through the natural birth canal.
Is it possible for a uterine rupture due to a scar?
After a conservative myomectomy (removal of uterine fibroids while preserving the uterus), after a previous cesarean section, i.e. in any case of a scar on the uterus, it may rupture during pregnancy or childbirth. According to foreign literature, the incidence of uterine rupture after a previous cesarean section is about 6%. Accurate data on the likelihood of uterine rupture due to a scar after myomectomy are not provided.
The likelihood of this complication is quite difficult to determine, since it is determined primarily by the individual characteristics of the uterine muscle tissue, which cannot be assessed. Patients with a uterine scar require more careful management of pregnancy, constant assessment of blood flow in the scar and its condition, timely development of a birth plan (vaginally or by cesarean section), timely hospitalization in antenatal departments, etc.
What to do if you have multiple uterine fibroids?
The issue of planning pregnancy in the presence of multiple uterine fibroids is quite complicated. In some cases, there may be several fibroid nodes of various sizes in the uterus, and removing them all can lead to virtually no healthy tissue remaining on the uterus.
In such cases, it is recommended to remove only those nodes that really interfere with pregnancy, i.e. located in such a way that they prevent the attachment of the embryo or large nodes that have a tendency to grow, which can complicate the course of pregnancy. After childbirth, you can subsequently remove the remaining myomatous nodes, or do this during a cesarean section.
It is not advisable to remove all nodes in preparation for pregnancy if there are a large number of them, since this can negatively affect the possibility of pregnancy, gestation and the course of labor.
What to do if you have multiple uterine fibroids?
When performing laparoscopy and conservative myomectomy, if the patient has infertility, it is mandatory to check the patency of the fallopian tubes, restore them, as well as perform hysteroscopy to exclude endometrial pathology and assess the condition of the uterine cavity after its suturing during surgery.
Causes of occurrence after surgery
Adhesions after uterine amputation are one of the most unpleasant consequences of the postoperative period. According to statistics, adhesions after surgery occur in more than 90% of women. The adhesive process, despite its apparent harmlessness, is a serious postoperative complication. The danger of developing an adhesive process is that it can lead to serious illnesses and cause unpleasant symptoms.
If the adhesions are extensive, they are defined by the term “adhesive disease.” Gynecologists say that it is necessary to differentiate physiological and pathological adhesive processes.
During hysterectomy, accompanied by amputation of the uterine body, connective tissue scars always appear. Such scars are physiological adhesions. However, if fibrous cords continue to grow and disrupt the functioning of neighboring organs, this pathology is called adhesive disease.
Fibrous cords are light in color and durable. In their structure, such adhesions resemble fibrous formations that connect organs.
The etiology and pathogenesis of adhesive disease have not been sufficiently studied. Typically, the appearance of adhesions is characteristic of large-scale operations involving amputation of several organs.
There may be several reasons for the formation. The formation of adhesions may be associated with the following factors:
- duration of the operation;
- volume of intervention and blood loss;
- the presence of surgical and postoperative bleeding, which contributes to the appearance of adhesive disease;
- infection in the period after surgery;
- genetic predisposition, manifested in the absence of an enzyme that resolves fibrin deposits;
- asthenic physique.
The actions of the gynecologist during the operation are essential in the formation of adhesions. It is important whether the incision was made correctly and the postoperative suture was applied.
Causes, symptoms, diagnosis of adhesions in the uterus
The peculiarity of the occurrence of adhesions is that they act as a kind of protectors of healthy tissues from the affected ones.
Causes of adhesions
No disease occurs without a cause or effect of something. Many factors can lead to the formation of adhesions. The main ones are:
- The presence and course of the inflammatory process in the pelvic organs. Due to the presence of inflammation, a substance called fibrin begins to be released in the uterus, which causes the walls of the organ to stick together. They look like thin threads. Next, the fibrin threads become overgrown with collagen protein fibers, which thickens them and makes them strong.
- Hormonal imbalances.
- Incorrect installation of the intrauterine device.
- Abortions and miscarriages, frozen pregnancies.
- Previous pelvic surgeries and subsequent treatment.
Symptoms when they occur
Adhesions after hysterectomy surgery are known to have symptoms. However, these symptoms of adhesive disease after hysterectomy are not always pronounced. Despite the fact that the severity of symptoms is individual, you can suspect adhesions after surgery to remove the uterus based on the following symptoms.
- Pain. The woman notices aching and nagging pain, which can be relieved by taking painkillers. It is noteworthy that pain can be both constant and periodic, and also reach significant intensity.
- Disturbances regarding urination and defecation. With adhesions, excretory function disorders are noted.
- Symptoms of gastrointestinal disorders. Quite often, adhesions after removal of the uterine body are manifested by flatulence and excessive intestinal motility.
- Increase in body temperature. Adhesions after hysterectomy can cause both high and low-grade fever.
- Postoperative scar pain. An important symptom indicating the presence of adhesive pathology is pain when palpating the scar, as well as its swelling and redness.
Symptoms of adhesions also include pain during sexual intercourse. In some cases, bloody discharge from the genital tract may occur. Despite the presence of symptoms, examination is necessary to confirm the diagnosis.
Degrees of adhesions
Based on the number and characteristics of adhesions, the disease is divided into three degrees.
- In the first degree, adhesions occupy a small area and do not extend into the fallopian tubes.
- In the second degree, the lesion reaches up to 70% of the entire area of the uterine cavity, covering its fundus, as well as the fallopian tubes.
- And the most difficult to treat and eliminate is the third degree of damage. It covers almost the entire uterine cavity.
Also, according to the degree of thickening of the adhesions, there are three forms of manifestation:
- The simplest and easiest form is the first. The adhesions have a thin base and are easily dissected using a hysteroscope.
- In the second form (medium), synechiae have a dense muscle structure. When removed and cut they bleed.
- The third form is the most severe. When removing, cutting adhesions is quite difficult. The structure is quite dense.
Diagnostic methods for identifying
Diagnosis of adhesive disease after amputation of the uterine body is difficult. This is due to the fact that in most cases, an accurate diagnosis is only possible during laparoscopy or abdominal surgery.
The presence of adhesions after hysterectomy can be suspected after analyzing the patient’s symptoms and medical history. It is possible to confirm adhesive pathology using basic diagnostic methods.
- Laboratory research. This is an additional examination method that involves a blood test; it helps to identify inflammation and assess the activity of fibrinolysis.
- Ultrasound of the abdominal and pelvic organs. This examination method allows us to assume, and in some situations, to identify the presence of adhesions after hysterectomy by determining the incorrect position of organs that are “tightened” by adhesions.
- X-ray of the intestines. The study is carried out using a contrast agent. This method is auxiliary, as it helps to assess both intestinal patency and narrowing of the lumen.
- Laparoscopy. This method is optimal for diagnosing and treating adhesions after hysterectomy surgery. The surgical process involves dissection and removal of adhesive formations.
Surgical tactics for treatment
Adhesive disease is treated primarily with surgical techniques. This is due to the fact that conservative methods are ineffective and are used for preventive purposes, for example, in the postoperative period. Drug treatment is also used to eliminate unpleasant symptoms.
To eliminate adhesions after removal of the uterus, doctors use two types of operations:
The operation using laparoscopy involves making several small punctures in the abdominal wall. These punctures are necessary for the use of special equipment during the operating period.
Laparoscopy has a number of advantages:
- dissection of adhesions is performed under the direct control of the optical system;
- tissue trauma is minimal;
- cutting of adhesions with special instruments followed by hemostasis;
- absence of symptoms such as severe pain and postoperative complications;
- the recovery stage takes several days;
- rapid disappearance of symptoms of adhesions;
- possibility of physical activity the next day after surgery.
Gynecologists note that laparotomy is rarely used in the treatment of adhesions that arise after amputation of the uterine body. Laparotomy is used mainly in the following situations.
- Lack of possibility of laparoscopic surgery.
- Symptoms of extensive adhesive disease in the peritoneum.
The surgical stages of laparotomy involve the use of an inferior midline approach. Then surgeons expand its top to fifteen to twenty centimeters. This tactic is necessary for a thorough examination of all organs and removal of adhesions.
Laparotomy is considered a traumatic operation. This is due to the fact that such an operation has a significant risk of operational and postoperative complications. Relapses often occur after laparotomy surgery, and the recovery period lasts about a month.
After the operation, the woman is recommended to regularly visit a doctor who monitors the progress of recovery. After surgical removal of adhesions, the possibility of recurrence is high.
Gynecologists advise following the recommendations of the treating doctor in the postoperative period and preventing the occurrence of adhesions. If you have reproductive plans, it is advisable to start planning a pregnancy after the end of the recovery period.
Prevention education
The risk of surgical and postoperative complications largely depends on the actions of the surgeon. In this regard, you should approach the choice of a doctor responsibly. The postoperative recovery period also depends on the progress of the hysterectomy.
Only absorbable thread should be used as material for suturing the incision. Hysterectomy is considered a fairly extensive and serious operation, and the threads are a foreign object - an antigen for the body. Over time, the threads become overgrown with connective tissue. Subsequently, the formation of adhesions begins. Accordingly, the nature of the adhesions also depends on the correct execution of the seam.
In the postoperative period after amputation of the uterine body, drug therapy is necessarily prescribed. The patient is recommended to take broad-spectrum antibiotics. These drugs prevent infection and inflammation. The use of anticoagulants is also advisable.
To eliminate symptoms after surgery, as well as to prevent adhesions, physical therapy is performed. In particular, electrophoresis destroys the formation of adhesions and reduces the severity of symptoms in the early postoperative stage.
After removal of the uterus by hysterectomy, the patient undergoes regular examinations, including pelvic ultrasound and gynecological examination.
Early motor activation of the patient after removal of the uterine body is essential. For example, walking may improve intestinal motility and reduce the risk of adhesions.
Surgical treatment involves following a proper diet. A woman should avoid spicy, salty and fried foods, as well as alcohol and carbonated drinks. An improper diet impairs digestion, which weakens intestinal motility.
After discharge from the hospital, a woman must follow the doctor’s instructions, in particular, take prescribed medications and undergo physiotherapeutic treatment. In some cases, you can use folk remedies to prevent adhesions after surgery to remove the uterus.
Rehabilitation period
The postoperative period after removal of uterine fibroids can last a varying amount of time, depending on the type of intervention. After surgery, the patient is not recommended to remain on long-term bed rest. The first rise from the bed is recommended 10-12 hours after the operation; you need to start moving slowly around the clinic room. This is an excellent prevention of congestive processes in the pelvic area, as well as an effective way to help prevent further relapse of the disease.
If a woman’s well-being does not deteriorate, she is not bothered by nausea or vomiting, which can be caused by pain relief, they must begin to introduce drinking into the patient’s diet. This could be a few sips of still mineral water, unsweetened tea, compote or fruit drink.
IMPORTANT! The recommendation for a speedy recovery also concerns nutrition - food should be as simple and natural as possible. It is best if it is liquid porridge, lean broth, stewed or boiled vegetables. It is recommended to focus on products rich in iron and protein compounds - lean meats, liver, fish, pomegranates. This will help relieve irritation of the rectum and normalize stool.
After removal of uterine fibroids, it is important to remember a few rules:
- A diet will help you recover faster - you should stop eating baked goods and wheat bread, legumes, white cabbage, and strong black coffee for a while.
- A woman needs to ensure sexual rest by eliminating sex from her life for 8-12 weeks.
- You cannot engage in sports or any type of physical activity, restrictions must be observed for at least 12 weeks.
- Under no circumstances should the uterus be overcooled or overheated; this will help prevent complications after surgery.
Mandatory elements during recovery include regular walking in the fresh air, physiotherapy, and special therapeutic exercises. It is very useful to wear special shapewear or a bandage - this will help muscle tissue recover faster and relieve discomfort.
To restore hormonal levels in the female body, hormonal medications are used. Most often, the use of Diferelin, Janine, as well as the dietary supplement Wobenzym is recommended.
Questions and answers on: adhesions after hysterectomy
Hello dear doctors! 07/01/2009 at the age of 47 years, I underwent surgery for grade 3 cervical dysplasia. (The focus was in the cervix measuring 05.*1 cm) - extrepation of the cervix with appendages. There was no menopause and the ovaries were healthy, but the gynecologist-oncologist before the operation advised me to urgently remove the ovaries as well, because... Considering their experience and my pathology, I could end up back on their operating table with the same pathology or even worse. They didn’t leave me any other options and I agreed. Which I repent of now. After the operation I felt more or less satisfactory. But after 8 months, pain appeared in the lower abdomen, a feeling of heaviness. The pain radiates to the sacrum and rectum. I no longer feel the urge to defecate. I feel some kind of unpleasant sensation, and during a digital examination I feel that the ampulla of the rectum is full of feces and I feel the bulging of the vaginal stump into the rectum. Weakness, fatigue. These pains have been tormenting me for a year now. She became nervous and irritable. I’m already thinking about suicide (I wish I could take sleeping pills and fall asleep, forget about this pain). I have been taking Angelique for 7 months because... there were hot flashes and increased glucose, cholesterol and bladder problems. It got a little better. On CT scan of the pelvis - Condition after removal of the uterus and appendages. Vaginal stump with clear, uneven contours, surrounding tissue with fibrous changes and “small” calcifications. The bladder is significantly full, of normal shape with clear, even contours, the contents are homogeneous. Ultrasound of the pelvic organs: There is an adhesive process in the pelvis, no visible formations were detected. The bladder has clear, even contours, the walls are compacted, without visible additional formations. Volume of initial urine: -350ml. The volume of residual urine is 55 ml. Irriography - With the retrograde administration of a liquid barium suspension, all sections of the colon were performed up to the dome of the cecum. The localization of the loops of the sigma and the descending colon is disturbed. The descending colon is displaced medially, forms a knee-shaped bend, the sigma, against the background of its lengthening, forms multiple looped bends and kinks, the displacement of the loops is sharply limited and painful. In the descending colon, in the sigma, the haustration is smoothed, uneven, the folds of the mucous membrane are moderately thickened. Throughout the rest of the colon, symmetrical haustration is preserved. No organic narrowings or filling defects were detected. conclusion: R signs of a violation of the anatomical localization of the distal parts of the colon as an indirect sign of adhesive disease, signs of chronic colitis. EGDS - The esophagus is freely passable. The mucous membrane is pink. The cardinal sphincter closes. In the stomach there is a moderate amount of turbid contents, an admixture of mucus. The gastric mucosa is pink and swollen. The pyloric sphincter is concentric. The duodenal bulb 12 is not deformed, the mucosa is pink, it looks like “mannol grains!” The post-bulb part is pink. Conclusion: superficial gastritis. Moderate inflammation. Indirect signs of pancreatitis. Colonoscopy - perianal area is clean. Colonoscopy was performed to the splenic angle of the colon. The mucous membrane is pink throughout, the vascular pattern is not changed. Peristalsis is uniform. Conclusion: no signs of inflammation were detected. A few days ago I went for a consultation with a surgeon and gynecologist regarding adhesive disease. The gynecologist prescribed electrophoresis on the lower abdomen with lidase (1.5 years have passed since the operation). Will lidase help now? I've heard about Longidase. What is it? Does it help? The surgeon looked at my examination results and sent me to an oncologist: let them figure out what these “small” calcifications on the peritoneum are! If there is an adhesive process, then we will wait until OKN occurs. Then we will operate on emergency indications. WOW! So we have to wait for OKN or peritonitis or intestinal necrosis! What if the ambulance doesn’t arrive on time or brings you to a drunken surgeon during the holidays? What then! Die! 2 days ago I went to another surgeon because... I have no strength to endure the pain. A female surgeon looked at all the examinations and my stomach and diagnosed adhesive disease of the abdominal cavity. Dolichosigma. Colonoptosis. Coccygodenia. Prescribed Movalis, suppositories. Milgama No. 10 Magnetotherapy for the cross. department. No. 10. Electrophoresis with novocaine No. 10. She advised me to go for a consultation with a proctologist - maybe he’s talking about prolapse of the small intestine? I'm tired of doctors, medications and pain. I don't want to live! But it seems like I’m not old yet, and I need to work a lot, I have a loan from the bank. But I can’t work.
What are adhesions
Doctors also call extensive adhesions of internal organs adhesive disease. However, it is important to distinguish the physiological process of adhesion formation from the pathological one.
Removal of the uterus (hysterectomy) is always accompanied by the formation of connective tissue scars at the sites of scars and incisions. The scars that form are physiological adhesions. Scarring of the wound gradually stops, due to which the normal functioning of the organs is restored, and the symptoms of inflammation disappear.
Important! The process of formation of adhesions (or scars) after removal of the uterus is a normal physiological condition that has nothing to do with pathology. If the formation of connective tissue does not stop, and fibrous cords grow and grow into other internal organs, this is a pathology called adhesive disease. It has its own symptoms and requires serious medical intervention.
These pathological fibrous cords have a whitish tint. They look like fibrous formations connecting internal organs. The strength of the cords is high, which is why it is necessary to resort to repeated surgery to remove them.
Classification
Adhesions in the uterus are classified according to different criteria. Let's focus on 2 types of classifications.
According to the volume of filling of the uterine cavity by the adhesive process:
The second classification reflects the histological characteristics of adhesions and severity:
- Mild degree - thin cobwebs from the basal layer. They are easily torn with a hysteroscope tube.
- Moderate severity – fibromuscular adhesions. They are covered with endometrium and bleed when cut.
- Severe degree – connective tissue. Their separation is difficult. They don't bleed.
Reasons for the formation of adhesions after removal of the uterus
In the body, adhesions occur mainly only after extensive operations that require the removal of one or two organs at once. The reasons for their occurrence are varied and depend on a number of factors:
- How long did the operation take?
- Scope of surgery.
- Volume of blood loss.
- Internal bleeding in the postoperative period. In this case, active resorption of blood accumulated in the abdominal cavity occurs, and this predisposes to the occurrence of adhesions.
- Wound infection in the postoperative period.
- Genetic predisposition. This is due to the fact that a genetically predisposed organism does not produce a special enzyme capable of dissolving fibrin deposits, which ultimately leads to the appearance of symptoms of adhesive disease.
- People of asthenic physique.
- In addition, the occurrence of adhesions depends on the actions of the surgeon himself. What is important here is how correctly the incision was made, what suture materials were used, and how professionally the suture itself was applied.
- There are cases where surgeons left foreign objects in the abdominal cavity. This also predisposes to the development of adhesions after hysterectomy and symptoms of adhesive disease.
What to do if adhesions form after laparoscopy
Changing food
If there is an adhesive process after surgery using the laparoscopic method, a change in diet is indicated to help eliminate the pathology as quickly as possible. Spicy, fried and fatty foods are excluded from the diet, as well as:
- products that increase gas formation in the intestines;
- alcohol;
- hot and fatty sauces;
- marinated and smoked dishes;
- canned food
The menu for spikes should consist of fermented milk products, lean soups, low-fat meat and fish dishes, chicken eggs, fruits and vegetables, and various cereals. It is optimal to eat small meals five to six times a day.
To avoid the development of adhesions, it is recommended to use an anti-adhesion gel, for example, Mesogel. It is rubbed into the skin in a thin layer. You can perform special exercises aimed at eliminating pathology. You can learn more about exercises against adhesions HERE.
Adhesion therapy
If the pathology is asymptomatic, conservative therapy is indicated, involving the use of medications and physiotherapeutic procedures. If these methods are ineffective, then relaparoscopy is performed at the patient’s request.
The chronic painful form is usually treated conservatively, including by local treatment of the affected tissue. Physiotherapy and electrophoresis procedures using absorbable agents (iodides and lidase) are practiced. Drugs are prescribed to relieve pain and other symptoms of pathology.
Laparoscopic removal of adhesions
Dissection of adhesions is carried out using laparoscopic access.
In this case, three incisions (no more than a few millimeters in size) are made on the woman’s stomach. During the process of manipulation, the normal relationship between the organs of the reproductive system is restored, adhesions are removed, and a new hole is formed in the fallopian tube to replace the sealed one. Methods for removing adhesions:
- laser therapy, in which adhesions after removal of the uterus and ovaries or other surgery are cut with a laser;
- aquadissection – problematic tissues are removed using water supplied under pressure;
- electrosurgery, in which an electric knife is used to eliminate adhesions in the pelvis.
Symptoms of adhesions after surgery
You can suspect adhesive disease in a woman who has recently had her uterus removed by the following symptoms:
- Aching or nagging pain in the lower abdomen, forcing you to take an antalgic (forced) position. The pain can be constant or periodic and reach high intensity.
- Retention and other disorders of urination and defecation, up to the absence of urine and feces.
- Symptoms of dyspeptic disorders: pain throughout the abdomen, flatulence and gas formation, “sheep feces”, a feeling of increased intestinal motility and others.
- Low-grade or febrile body temperature (increase to 38-40 C).
- A feeling of severe pain when palpating the postoperative scar, its redness and swelling.
- Pain during intercourse. Vaginal discharge of a bloody nature.
- If several weeks have passed since the removal of the uterus, then if these symptoms appear, you should immediately contact your doctor (gynecologist).
Important! Symptoms of adhesive disease are nonspecific. This means that if a woman makes such complaints, then not a single qualified doctor can say with complete confidence that she has formed adhesions in the pelvis. To confirm the diagnosis, instrumental and laboratory examination methods are required.
The doctor told me that adhesions can cause intestinal obstruction. What is this? How dangerous is this?
Adhesions can harm health because they put pressure on different internal organs and because they glue internal organs together, limiting their natural mobility.
By pressing on the small intestine, adhesions can block its lumen and lead to the fact that digested food cannot move through the intestines and begins to accumulate in it, and the intestines themselves begin to swell and become inflamed. In medicine, this condition is called intestinal obstruction.
According to some studies, the probability of developing intestinal obstruction after various operations during which adhesions formed is about 0.15%.
The following symptoms may indicate the development of intestinal obstruction associated with adhesions:
If you notice similar symptoms, consult a doctor immediately. |
Diagnosis of adhesions in the postoperative period
A preliminary diagnosis is made after a thorough collection of medical history, patient complaints and symptoms of the disease. To confirm the presence of adhesions, the doctor prescribes an additional examination:
- General blood analysis. Necessary to check whether you have inflammation in the body. Also evaluate the activity of the fibrinolytic system of the blood.
- Ultrasound of the abdominal and pelvic cavity. A visual examination method helps to say with a 100% guarantee whether there is an adhesive process in the pelvis after hysterectomy.
- X-ray examination of the intestines using contrast (coloring) substances. An auxiliary method that allows one to judge the patency of the intestine and the degree of narrowing of its lumen.
- Laparoscopic diagnostics are also used, during which individual adhesive formations are dissected and removed, and the issue of repeated surgical intervention is also decided.
Causes
Adhesions in the uterus have been known to doctors for a long time, but the first to give them clinical significance was only in 1948 by a doctor named Asherman.
Since then, the presence of adhesions in the uterus and the problems associated with them, in addition to the second name “synechia”, have received another name – Asherman’s syndrome. It was found that adhesions in the uterus occur with greater frequency due to:
- Undeveloped pregnancy.
- Uncompleted abortion.
- Bubble drift.
- Bleeding after childbirth.
- Remains of the fertilized egg after a medical abortion.
- Application of hemostatic sutures to the uterus.
- Tuberculosis of the uterus.
- Radiation therapy.
- Curettage of the uterine cavity. Moreover, repeated curettage increased the risk of adhesions.
There is no single theory for the occurrence of adhesions in the uterus. But at the same time, 2 theories occupy the main positions. Thus, the traumatic theory suggests that during surgical interventions in the cavity, the basal layer is damaged, from the cells of which a new endometrium appears with each new cycle. The damaged basal layer is represented by islands of layers of mesothelial cells. The production of fine-fibrous synechiae begins, gradually filling the uterine cavity. After 5–7 days, re-epithelialization ends.
Adherents of the infectious theory believe that against the background of anti-inflammatory reactions occurring in the uterus that accompany any inflammatory process, the production of cytokines and other biologically active substances increases. This disrupts microcirculation, against the background of which exudation increases, and a protein, fibrin, begins to be deposited, from which adhesions are formed.
Surgical treatment of adhesions
Mostly adhesive disease is treated surgically. This is due to the fact that conservative treatment is not effective; it is used only as prophylaxis in the postoperative period and to relieve symptoms of the disease.
There are 2 types of operations:
- Laparoscopic surgery. It is carried out using special fiber optic technology. In this case, 2-3 small incisions are made on the skin of the anterior abdominal wall, and then the abdominal wall is pierced in these places. These punctures provide access to the abdominal cavity. The advantage of this operation is that the dissection of adhesions is carried out under the control of an optical system, with minimal trauma to internal organs. Using special laparoscopic instruments, fibrous cords are cut, followed by hemostasis. Pain and complications after such surgery are extremely rare. The recovery period takes several days, the symptoms of the adhesive process disappear almost immediately, and physical activity is possible the very next day after the operation.
- Laparotomy. Shown in two situations:
- There is no possibility of laparoscopic surgery.
- The presence of symptoms of extensive adhesions in the abdominal cavity.
In this case, first use the lower middle access, and then expand it upward to 15-20 cm. This is done in order to carefully examine all organs and remove overgrown adhesions. This operation is highly traumatic and has a risk of postoperative complications or relapse of the disease. The recovery period takes about two weeks.
After the operation of dissection of adhesions, it is necessary to constantly visit the attending physician to monitor the processes occurring in the pelvis
Important! No doctor can give a complete guarantee that adhesive disease will not return to you again. Removing adhesions is the same operation as removing the uterus, which means fibrous cords between organs can form again. To prevent this from happening, follow your doctor’s recommendations in the postoperative period and prevent relapse of the disease.
Sex after ectopic pregnancy
Regardless of how many days you are discharged after tubal surgery, you must maintain sexual rest during the recovery period. It is necessary for a complete recovery. Anal and vaginal sex after ectopic pregnancy surgery is allowed for at least a month.
You can begin sexual activity only if there are no complications and you feel well. It takes time for the body to fully recover from an ectopic pregnancy. Otherwise, treatment may be delayed.
Avoid sudden movements that cause discomfort. Choose sex positions more carefully and increase the intensity gradually. It is important to protect yourself from sexually transmitted infections and exclude pregnancy.
Oral medications plus condoms
Contraception methods
It is best to use both a condom and oral medications after an ectopic pregnancy. The former will protect against infection, and the latter will prevent conception. This way you will be able to completely protect your body.
Oral contraceptives are taken for at least a year after termination of an ectopic pregnancy. The drugs protect against conception and reduce the risk of genital inflammation. After 12 months of taking contraceptives, the likelihood of contracting such diseases decreases by 50–70%.
Prevention of adhesions formation
If you are scheduled to have a hysterectomy, choose your surgeon carefully. The course of the postoperative period largely depends on it.
What will the doctor do?
To close the wound, only absorbable surgical suture material is used. This is necessary because a hysterectomy is a large and highly traumatic operation. Threads are a foreign body that will become overgrown with connective tissue and subsequently form adhesions.
Professionally applies a suture when the edges of the wound are in contact with each other throughout.
Drug prevention of adhesive disease in the postoperative period. The doctor prescribes broad-spectrum antibiotics (to prevent infection, suppress inflammation), and anticoagulants.
Early prescription of physiotherapy with electrophoresis of enzymes that destroy fibrin (lidase, hyaluronidase and others). They destroy dense adhesive formations, which contributes to the rapid fading of the symptoms of the disease.
Dynamic observation after surgery, careful monitoring of the condition of the pelvic organs using ultrasound.
What should you do
To prevent adhesions, early physical activity after hysterectomy is important. The fact is that while walking, intestinal motility improves, which prevents the development of adhesions.
The second point is diet. Avoid salty, spicy, fried foods, alcohol, carbonated drinks. They disrupt digestion and intestinal motility weakens. You need to eat up to 6-8 times a day in fractional small portions. This will not overload the intestines, which means it will not become overtightened with fibrous deposits.
Follow your doctor's recommendations. After leaving the hospital, it is important to continue taking medications and doing physical therapy.
As for traditional methods of treatment, they can be used as an addition to drug therapy and only after consultation with the attending physician. For the prevention and treatment of adhesions in folk medicine, infusions and decoctions of plantain, dill, flax seeds, St. John's wort, and aloe leaves are used.
FOLK METHODS OF COMBATING SPIKES
Traditional medicine is used as an additional measure to help combat adhesions. It cannot be the only treatment method, because its effectiveness in comparison with “classical” treatment methods is low, but it is applicable as a maintenance therapy aimed at combating inflammation and general strengthening of the body.
- Crushed aloe leaves are mixed with a small amount of honey and milk, after which the mixture is taken one tablespoon at a time three times a day.
- Dried St. John's wort is poured with a glass of boiling water and boiled over moderate heat for a quarter of an hour. The decoction is taken three times a day, about a quarter glass.
- A tablespoon of milk thistle seeds is poured into half a glass of boiling water and boiled for ten minutes. The decoction is filtered, cooled and taken warm, a tablespoon three or more times a day.
Important: Before taking these products, make sure that you are not intolerant to their components.
Let's sum it up
Adhesive disease disrupts the physiological functioning of all abdominal organs. It is a consequence of highly traumatic operations. Advanced forms of adhesive disease can only be treated surgically, but this also causes harm to the body. To prevent this from happening, it is necessary to follow the recommendations of the attending physician in the postoperative period and prevent relapse of the disease. When the first symptoms appear indicating the presence of adhesions in the body, you should immediately consult a doctor for consultation and subsequent diagnosis.
Doctors' opinions on rehabilitation
Specialists know how to restore the body, how long it takes, and what needs to be done for this. They advise undergoing diagnostic tests every month to monitor your health. Doctors may refer you for additional examinations to specialists.
It is important to take care of yourself, avoid baths and saunas, alcohol, heavy physical activity and stress. The more time passes before conception, the better. It is necessary to prepare the body for pregnancy as much as possible to prevent relapse.
About the author : Borovikova Olga
Source