The period from the moment of puberty of a girl until the decline of reproductive function is necessarily accompanied by secretion from the vagina. The most commonly observed mucous discharge in women is snot, which under certain conditions is considered normal. But disorders that require therapy cannot be ruled out.
Characteristics of normal discharge in women
The release of a substance from the genital tract can be attributed to a cleansing mechanism that removes “waste materials” from the reproductive organs. The composition of leucorrhoea is:
- Dead cells that are spontaneously rejected by the uterus and excreted through the fallopian tubes and vagina.
- Non-inflammatory effusion that accumulates in the blood and lymphatic vessels.
- Various microorganisms that form microflora, but have become obsolete.
- Moisturizing, enveloping and protecting mucus produced by the cervix and “washing” the uterine cavities (cervical fluid).
Vaginal discharge like snot should not be a cause for concern if it:
- transparent (colorless);
- have whitish veins;
- leave a yellow mark on the panty liner after drying;
- odorless or slightly sour;
- do not cause discomfort (burning, itching, pain);
- viscous, lump-free and dense clots of pus;
- several hours or days are noted.
Based on the norm established by gynecologists, the volume of secretions of clear mucus without third-party aromas should not exceed 4 ml per day (one teaspoon). If the threshold is slightly exceeded, but no changes in other parameters are observed, then this phenomenon can be attributed to the peculiarities of the functioning of the reproductive organs.
The photo shows normal female mucus discharge:
White mucus discharge Discharge like snot Clear discharge White mucous discharge
Physiological causes of discharge clear as snot
The presence of very abundant mucous discharge in girls is not normal. This is due to the fact that before reaching puberty, the egg is in the stage of formation and active development, which means that the hormone estrogen is just preparing for production.
This substance is a harbinger of the formation of the menstrual cycle. After the girl has reproductively “formed” and become a girl, she will be constantly present, changing intensity and saturation depending on the phases of the cycle.
Mucus discharge after and before menstruation
The appearance and volume of discharge depends on the predominance of a particular hormone in a particular phase of the cycle. Such secretion is allowed before and after menstruation.
- At the beginning of the menstrual cycle after monthly blood loss, most girls notice viscous sticky mucus on the pad, sometimes mixed with blood, so a pink or light red tint is possible. Heavy mucous discharge after a scanty period sometimes means pregnancy.
- In the middle of the cycle, ovulation occurs, which is accompanied by a maximum amount of estrogen. This hormone makes the discharge abundant and also reduces its viscosity to facilitate the path of sperm to the egg, while at the same time it can pull the lower abdomen. However, not all women have a thin mucus consistency at this time.
- Towards the end of the menstrual cycle, the hormonal background stabilizes, there is less and less secretion, it becomes transparent, sometimes slightly white, and the consistency resembles a cream or even jellied meat. A few days before your period, the secretion may appear again, so discharge like clear mucus stretching between the fingers is not excluded.
Probability of conception and pregnancy
If there is a delay, and instead of menstruation there is a discharge very similar to snot, then pregnancy cannot be ruled out. The level of the hormone prolactin increases in the body, causing thicker secretion, which protects the woman’s reproductive system and fetus from harmful bacteria and infections. At this time, brown or pink mucus from the vagina is also possible, indicating the fixation of the fertilized egg in the uterine cavity.
In the second trimester (from 14 to 27 weeks), a small amount of such discharge indicates a normal course of the gestation period. When their volume increases, they flow like water, which means there is a threat of premature birth, especially if blood clots are present.
But in the later stages (9th month), the appearance of copious and highly viscous discharge during pregnancy is most often associated with the passage of a mucus plug, which indicates the approach of labor. Small blood clots may be present, but significant blood loss requires immediate medical attention.
After the baby is born
First, blood is present in the secretion, which indicates the cleansing of the body. After 6–8 weeks, mucous discharge begins to appear, like snot with a liquid and transparent structure. If a woman is breastfeeding, the secretion becomes thicker due to increased prolactin, which also delays the onset of the first menstruation after pregnancy.
After operations
Surgery is often accompanied by postoperative bloody or brown secretion. After a while, it is replaced by mucus, indicating complete healing of all microdamages. Therefore, do not worry if such odorless and itchy secretion appears after these manipulations:
- radio wave cauterization of erosion;
- curettage procedure;
- C-section;
- artificial termination of pregnancy;
- removal of tumors;
- conization of the cervix.
At first there will be red or brown copious discharge, which will gradually become transparent and thicken, resembling mucus. Some pain is possible, but it goes away with time.
Menopause
During menopause, stringy discharge in women like snot is not a sign of health problems if there is no itching, burning or redness. Later, a woman in menopause observes less and less vaginal secretion due to low production of sex hormones.
If a woman takes hormonal medications, they can affect the vaginal secretion, increase its quantity or slightly change the consistency, but no more.
Intimacy and change of sexual partner
Both before and directly during sexual intercourse, a woman’s arousal is accompanied by the production of vaginal secretions. Stimulated by brain impulses triggered by an intimate moment, the uterus produces a large amount of clear, mucous, odorless vaginal discharge called “lubricant.” This substance helps prevent injury to internal surfaces and avoid discomfort.
After the end of intercourse, the body is rebuilt, which means that the fluids change qualitative and quantitative properties. Intimacy that occurs with the use of a condom entails the production of a creamy substance of white or faded yellowish color. After several hours, the secretion loses color, acquiring rich shades and gaining noticeable thickness.
How long does the discharge last after childbirth?
Despite the fact that the exact answer to how long bleeding lasts after childbirth is always individual, normally it lasts on average from 6 to 8 weeks. Regardless of how many days after birth the discharge occurs, it is important that over time it becomes more and more scanty.
How long discharge lasts after childbirth depends on many things, so not everyone has the same amount of time. How long the discharge continues depends on the physiology of the body, the intensity of uterine contractions, the characteristics of delivery and a number of other points. Also, how long postpartum discharge lasts depends on whether the woman is breastfeeding . At the same time, how long the discharge with blood stains lasts after childbirth is an indicator of whether the young mother’s body is recovering normally.
The actual question is how long the discharge lasts after a cesarean section . It should be understood that this is a surgical operation, and the body’s recovery after it takes a longer period. Accordingly, the duration of lochia after cesarean section may be longer. However, how long the discharge lasts after a cesarean section largely depends on how successful the operation was and whether complications develop after it. As a rule, such discharge should last about 8 weeks.
A woman should be wary of smelly discharge after a caesarean section, as this may indicate the development of an inflammatory process. You also need to track how long the discharge lasts so as not to miss the symptoms of pathology. If you have any suspicions, it is better to consult a doctor.
Characteristics and causes of pathological discharge
Often, mucus secretion in women that does not correspond to the norm is caused by the following problems:
- infection in the vagina;
- chronic fungal diseases;
- consequences of the operation;
- incorrectly selected hormonal therapy;
- decreased immunity;
- changes in vaginal microflora;
- pathological processes in the reproductive system.
In each individual case, in addition to the secreted mucus, the woman will note additional symptoms that cause discomfort. But in the early stages of diseases it may be absent, and then the first signal will be precisely modified secretion.
A direct indication of health problems is vaginal discharge, which has the following features:
- rich color (yellow, green, brown, scarlet);
- long duration (more than three or four days are observed);
- heterogeneous consistency (lumps, blood clots, pieces of pus);
- a sharp increase in temperature;
- general malaise;
- rashes on the external genitalia;
- systematic burning and itching in the perineal area;
- pain in the lower back and abdomen;
- foamy or curdled consistency;
- discomfort while washing.
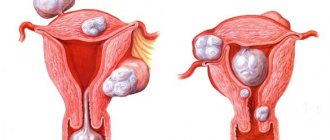
The photo shows examples of pathological secretions:
Bloody mucus Orange discharge Bloody discharge Yellow discharge
Constant discharge in significant quantities, even without discomfort, indicates disturbances in the microflora of a woman’s vagina. Without timely diagnosis and properly selected treatment, protective functions are reduced, creating favorable conditions for various infectious and fungal diseases.
Snot-like discharge based on shade
No less than the volume and consistency of the secretion, its color also indicates the processes occurring in the woman’s genital organs.
Transparent with green particles
The discharge indicates the presence of an advanced sexually transmitted infection. Accompanied by a characteristic putrid odor, burning and itching in the perineal area. Sometimes they are supplemented by pain in the lower abdomen and allergic rashes in the armpits.
White
White, odorless mucous discharge is not caused by diseases of the reproductive system, and may well be a physiological norm if we are talking about the following:
- the beginning of the ovaries (puberty);
- a specific segment of the monthly cycle;
- discharge during sexual arousal and intercourse;
- suffered stress;
- sudden climate change;
- reaction to an intimate hygiene product;
- use of HRT or OK;
- pregnancy;
- preparing the body for childbirth;
- breastfeeding;
- menopause
The appearance of a rich white color, a cheesy consistency and an unpleasant odor indicates thrush. A woman in this condition feels itching and burning, and swelling of the external genital organs is also possible.
Chronic candidiasis is dangerous because the symptoms are not systematic, appearing only during exacerbations, against the background of weak immunity or prolonged treatment with antibiotics. Particular caution should be exercised by pregnant women who are uncomfortable with the appearance of white snot-like discharge, since thrush can be transmitted to the baby during childbirth.
Yellow
Why do women secrete yellow mucus like in the photo above? Often their occurrence indicates infectious diseases or inflammatory processes. This condition is characterized by:
- large amounts of secretion and clots;
- presence of pus;
- increased body temperature;
- foamy consistency;
- cutting pain in the abdomen or lower back;
- strong unpleasant odor (rot, fish);
- pain when urinating (suspicion of cystitis);
- discomfort during sex and yellow discharge after sex that does not go away on its own.
Doctors also associate the yellow tint of secretion with allergies and the initial period of taking OCs.
Yellow-green and gray
Each type of infectious disease is accompanied by characteristic vaginal secretion:
- Copious amounts of gray, snot-like substance that smells like fish (hardrenellosis).
- Jelly-like or watery secretion due to the appearance of blisters on the labia (genital herpes).
- A large amount of yellowish or greenish discharge with pus (trichomoniasis).
- The presence of clear mucus with a very unpleasant and pungent aroma (ureaplasmosis).
- Abundant mucopurulent secretion with or without odor (chlamydia).
Transparent discharge with blood like snot and no odor
Most often, pink color indicates the following:
- the beginning or end of the menstrual cycle;
- endometritis, in the presence of an unpleasant odor;
- cervical erosion at an early stage;
- internal microtrauma due to improper placement of the coil, tampon, or during intimacy;
- threat of miscarriage, combined with nagging pain in the lower abdomen and sharp spasms in the lower back during pregnancy;
- tumor development when mucous discharge with blood streaks is present in menopause.
Brown
During menstruation, female discharge with a brown tint resembling snot is a physiological norm, but prolonged ichor mixed with mucus may indicate the following conditions:
- internal bleeding;
- acute inflammatory process in the uterus;
- pathology of blood and lymphatic vessels in the internal cavities or fallopian tubes;
- endometritis during an exacerbation;
- polyps;
- spiral rejection;
- ectopic pregnancy;
- the threat of miscarriage at an early stage of the gestation period and premature placental abruption at a later stage.
A manifestation of a physiological norm, indicating the correct functioning of the reproductive organs - transparent and mucous discharge. If such a secretion is burdened by pain, an unpleasant odor, or volumes that are many times higher than normal, this is a serious reason to contact a specialist. Such manifestations can act as symptoms of sexually transmitted diseases or serious pathologies of the uterus that require curettage or cleaning.
A woman’s discharge is normal if it does not cause her discomfort and there are no deviations in the nature of the menstrual cycle. Any change in the color, volume, or smell of discharge is perceived as a sign of disease. But in some cases this is not a pathology. Therefore, it is important to know when to go to the doctor immediately, and when to take changes calmly. If clear, snot-like discharge appears, you need to pay attention not only to its color, but also to the smell and consistency, and if in doubt, consult a doctor immediately.
- Discharge during pregnancy
- Discharge after childbirth
- Discharge during menopause
- Causes of pathological leucorrhoea that resembles snot
- Bloody discharge
- Mucous leucorrhoea with unusual symptoms
When should you see a doctor?
Usually, mucous discharge (it is quite thick and stretchy, transparent or slightly milky in color) is considered to be a variant of the norm, because in a woman it can take on a different character depending on the phase of the menstrual cycle.
If you ignore this symptom and do not seek advice from a specialist in time, you may miss the onset of the development of any pathology:
- Cervical erosions;
- Sexually transmitted infections;
- Cervical oncology;
- Inflammation of the appendages (fallopian tubes, ovaries);
- Infertility or difficulty conceiving.
All complications can be avoided if you seek help in time. A visit to the gynecologist should not be postponed. If cervical erosion develops or genital infections appear, then it is necessary to be examined as early as possible. Only if the disease is detected in a timely manner is effective treatment possible.
In the postpartum period, it is very important to observe the rules of personal hygiene. The open wound surface of the uterus, and in some cases the sutures on the cervix or perineum, is an excellent breeding ground for the life of various microorganisms; it is humid and warm there. Inflammatory processes in the uterus or vagina develop very quickly. This is why it is so important for women to keep their external genitalia clean.
What discharge is normal?
Physiological vaginal discharge plays an important role in a woman’s body. They moisturize the vagina, protecting its surface from damage during sexual intercourse. An important function of leucorrhoea is to maintain a normal bacterial environment in the vagina and acidity necessary to prevent the penetration of pathogenic microorganisms into the uterus.
Leucorrhoea consists of mucus produced by the glands of the cervix and the vestibule of the vagina, and it also contains fluids that seep through the walls of this organ from the blood and lymphatic vessels. Normal mucus resembles the consistency of snot. Its density and transparency depend on the content of proteins and mucins (proteins whose molecules contain polysaccharide chains).
Normally, snot-like discharge should have the following indicators:
- They should be transparent, slightly white or beige in color.
- They should not have an unpleasant odor. A slightly acidic aroma may be present due to the presence of beneficial lactobacilli in the vaginal microflora, which prevent the spread of infection.
- The mucus should not foam, contain lumps or blood.
In addition, leucorrhoea should not be too abundant, causing irritation of the vulva and perineum, itching and burning in the vagina.
Physiological etiology
The so-called “white” lochia begins 7-10 days after birth. They are transparent or white, stretchy. Also, many women compare them to snot. There shouldn’t be any unpleasant odor, much less a high temperature!
The main cause of mucous discharge is fluid that passes through the blood vessels and lymph nodes:
- Uterine cells are capable of secreting transudate;
- During ovulation, mucus leaves the cervical canal;
- The cervix has the ability to secrete.
It is noted that the cells are especially active in the second phase of the menstrual cycle, at the time of ovulation and a few days before it. This happens under the influence of hormones. This ensures better lubrication and the environment in the vagina becomes less aggressive for sperm. The mucus that clogged the cervical canal and cervix in the first half of the cycle begins to move away and is released. All these are necessary conditions provided by nature for fertilization.
It is possible that the mucus that appeared in the discharge may either remain there or disappear when the postpartum period ends. The processes occurring in the body of each woman are individual.
It was also revealed that the nature of the discharge depends on whether the woman is breastfeeding her newborn baby. Breastfeeding (without complementary foods) inhibits the processes in the brain responsible for regulating the menstrual cycle. Therefore, it is difficult to predict whether mucous discharge will stop or whether menstruation will begin.
When is the appearance of mucous leucorrhoea considered normal?
In women of reproductive age, the density of mucus changes during the menstrual cycle. This is caused by fluctuations in the ratio of the female sex hormones estrogen and progesterone. Immediately after menstruation, the density is maximum, a mucus plug forms in the cervix so that sperm cannot enter the uterus, and the mucous membrane in it is restored. Then, in the first phase of the cycle, the mucus gradually thins out, and by the time of ovulation it becomes liquid and viscous, reminiscent of snot. It is at this moment (in the middle of the cycle, when ovulation occurs) that the maximum opportunity arises for a mature egg to meet sperm and fertilization. Then the mucus thickens again.
At the entrance to the vagina there are the so-called Bartholin glands, which produce mucus to eliminate “vaginal dryness”. At the moment of sexual intercourse, the production of lubricant increases sharply, and the woman develops abundant, transparent leucorrhoea, stretching like snot.
Sometimes odorless mucous discharge may appear regardless of the phase of the cycle as an allergic reaction to any foods or medications. The sensitive reproductive system in women can react with the appearance of such leucorrhoea to a change in the environment and climate.
Note: Sometimes normal mucous secretions contain minor traces of blood, which quickly disappear. They appear at the time of ovulation (rupture of the follicle), as well as at the time of implantation of a fertilized egg into the mucous membrane of the uterus (endometrium. This is the so-called implantation bleeding. Bloody leucorrhoea can be normal in the first months after starting to take birth control pills or installing an IUD.
Discharge during pregnancy
The formation of mucous leucorrhoea is also possible during pregnancy, when a sharp change in hormonal levels occurs in the body. If abundant white mucus does not cause discomfort in a woman and does not contain blood, then its formation is considered normal. In the second trimester, the density of leucorrhoea increases and it becomes viscous.
The appearance of blood impurities means that for some reason there is a threat of miscarriage or premature labor begins. Blood may appear during an ectopic pregnancy.
Discharge after childbirth
After childbirth, the discharge gradually turns from copious bloody mucus, reminiscent of menstruation, into stretching, colorless, odorless snot. If a woman is breastfeeding, then she has scanty, thick, transparent, yellowish discharge. After the restoration of menstruation, the discharge takes on a normal appearance.
Discharge during menopause
During this period, hormonal changes occur due to the cessation of normal functioning of the ovaries. Normal mucous leucorrhoea becomes scanty. Vaginal dryness and thinning of the mucous membrane often lead to inflammatory and infectious processes in the genitals. In this case, pathological discharge appears, which disappears after appropriate treatment.
The danger is usually caused by spotting mucous leucorrhoea with blood. At this age, bleeding is most often a symptom of cancer.
Video: Normal and abnormal vaginal discharge
WHEN MUCUUS DISCHARGE IN WOMEN IS NOT THE NORMAL
If a woman or her sexual partner neglects the rules of hygiene, physiological discharge may give way to pathological discharge. Mucus or flakes that emit a sharp sour odor or the smell of rotten fish, are grayish, cheesy, foamy, greenish, yellow, brownish, too abundant - all this indicates a probable inflammatory process. Alternatively, to distinguish normal discharge from pathological ones, you need to insert a clean finger into the vagina and run it along the glass. Normal mucus is light and transparent. In all other cases, this is a pathology and the woman should immediately consult a doctor and undergo an examination.
A brown tint of mucus a day or two before and after menstruation in the absence of an unpleasant odor is most often considered normal. Dark staining may occur in the first months of using oral contraceptives, or as a reaction to a change in drug. Brown color of uterine mucus may indicate chronic endometritis, endometriosis, endometrial hyperplasia. Particularly dangerous are mucous brown or bloody discharge in women during pregnancy, which may indicate a threat of miscarriage.
WHAT TO DO IN SUCH A SITUATION
All doubts about your women's health need to be resolved in only one way: contact a competent gynecologist. Only a qualified specialist can distinguish an extreme version of the norm from a formidable pathology and, if necessary, prescribe treatment. Remember: our women's health does not forgive negligence and amateurishness.
A completely normal occurrence for women of productive age is clear discharge like snot. They are observed during the period when the egg has matured and is preparing to leave the follicles and proceed through the cavity of the fallopian tubes to the uterus.
This miracle of nature, which plays an important role in the reproduction of humanity, is called ovulation and, if a woman is able to produce offspring, she ovulates every month. The purpose of this process is the meeting of a mature egg with a sperm. If they meet, then a new life is conceived, but if not, then the egg dies and menstruation begins.
The process of ovulation can be accompanied not only by mucous transparent discharge such as snot, but also by pain in the lower abdomen, as well as pain or discomfort in the mammary glands, and increased sexual desire for a partner.
Vaginal discharge during ovulation is its most striking sign, by which you can easily determine favorable days for the birth of a new life. The secretions help maintain the life of the sperm that get there; it is a favorable environment for them; the slippery secretions help the sperm move towards the goal, fulfilling the task of nature.
Sometimes such discharge can be abundant and leave stains on the laundry. After ovulation ends, the discharge changes. Due to the decrease in the amount of estrogen, clear discharge is replaced by white discharge like snot, it becomes creamy, as a new hormone comes into play - prolactin.
Such discharge during and after ovulation is normal, but they should not be confused with pathological discharge, which is not associated with natural physiological processes, but may be a sign of some disease.
Vaginal discharge of various types may indicate infectious diseases. Therefore, it is important for any woman to distinguish one from the other. How can you tell the difference? Discharge during ovulation is usually viscous, clear and odorless. They may turn yellow when dry.
Discharge in the form of snot in itself is not a cause for concern, but if it has a specific smell, a more liquid or solid consistency, a greenish or gray color, is accompanied by pain in the lower abdomen or when urinating, itching in the vagina, then, most likely, These are signs of an infectious disease. In this case, you should immediately consult a doctor and advise your sexual partner to do the same.
You should not hope that everything will go away on its own or self-medicate. This is fraught with the transition of an infectious disease to a chronic one. Advanced forms of infectious diseases can lead to serious consequences for women, including infertility. And if at this moment you become pregnant, then infections can negatively affect the development of the unborn child.
It should be noted that thick, profuse discharge can be observed in a pregnant woman in the last weeks of her term. This may be due to the gradual release of the mucus plug, which forms during pregnancy in the cervix and just protects the unborn baby from various infections. This plug can come out entirely immediately before or during childbirth, but it can also come off gradually in large or even small parts. This is just a normal phenomenon and you shouldn’t be afraid of it.
But in cases where vaginal discharge is not a pregnant woman’s mucous plug and a sign of ovulation, you should definitely consult a doctor to find out the causes and possible treatment.
A woman should be attentive to her health, because she is a future or already accomplished mother who is responsible for her children, and therefore for herself.
A healthy woman is normally and should have.
Vaginal mucus is normal
- Normally, mucous discharge may be yellowish or slightly cloudy.
- Most often, white mucus is released from the vagina on the eve of ovulation.
- In the first half of the cycle, mucus from the vagina is thick and stretchy in small quantities.
- Thin and clear vaginal mucus may appear during sexual arousal.
- In the second half of the cycle, vaginal mucus is creamy and becomes larger before menstruation.
- Thick mucus from the vagina, which is secreted in yellowish clots, occurs after unprotected sex. After a few hours, this discharge is liquid and white in large quantities.
- After protected intercourse, a very small amount of white mucus comes out of the vagina.
- If mucus streaked with blood is released from the vagina at the end of the menstrual cycle, then this is a harbinger of the onset of menstruation.
- After childbirth, not only mucus comes from the vagina, but also sanguineous discharge -.
Mucus from the vagina in pathological processes
Mucus in various diseases can change color (from brown to greenish), it may have an unpleasant odor, the discharge can cause itching or irritation of the genital tract, and contain impurities of pus or blood.
The appearance of any vaginal discharge that cannot be called normal is a reason to consult a gynecologist.
A woman’s health is very important, because it is the representative of the “weaker” sex who plays the main role in childbirth. If discharge in the form of mucus appears in women, it is necessary to clearly understand which of them are pathological and which are normal. It is especially important to understand the factors that cause white, clear, or cheesy discharge.
Causes of pathological leucorrhoea that resembles snot
Signs of pathology are:
The cause of the pathology may be diseases of the genital organs caused by infection, the occurrence of inflammatory processes, and hormonal disorders in the body.
Bloody discharge
The appearance of bloody leucorrhoea indicates either injury to the mucous membranes of the vagina or vulva, or the formation of tumors in the genital organs, areas of inflammation with damage to blood vessels.
Diseases of the cervix (erosion, dysplasia, leukoplakia). All of them are associated with damage to the mucous membranes, the appearance of ulcers, cracks, and areas of keratinization on the surface of the cervix. They begin to bleed when walking or changing body position. Symptoms of pathologies are often the appearance of pain and bleeding during sexual intercourse. The causes of such diseases are hormonal disorders, damage to cervical tissue during childbirth, abortion, gynecological operations, and rough sexual intercourse.
Uterine fibroids. This is a benign tumor inside or on the outside of the uterus. The pathological development of tissues and blood vessels leads to the constant appearance of blood in the mucous leucorrhoea, which has nothing to do with menstruation and is not associated with the processes of the cycle.
Endometriosis is the abnormal development of the endometrium, pathological growth of the vascular network, swelling of the mucous membrane, throwing its particles into the ovaries, peritoneum and other organs. With this disease, blood clots and particles of damaged endometrium can be seen in the mucous secretions. Due to internal bleeding, they are usually brown in color. They can be either abundant or scanty (smearing).
Endometrial or cervical polyps are thin stalked formations that are easily damaged and bleed.
Malignant tumors of the uterus or ovaries. Streaks of blood and lumps appear due to tissue destruction.
Note: When benign or malignant neoplasms appear in the uterus, clear mucous discharge mixed with blood can turn into heavy intermenstrual uterine bleeding.
Such diseases usually appear when hormonal changes occur in the body associated with age, changes in physiological state, and the use of hormonal drugs.
Mucous leucorrhoea with unusual symptoms
The smell and color of the discharge, similar to snot, changes when inflammatory processes occur in the body after surgery, as a result of decreased immunity, hypothermia, disruption of the vaginal microflora due to taking antibiotics. The peculiarity of pathological discharge is that it appears without any connection with the processes of the cycle and continues after menstruation, when the mucus should be the thickest and produced in an insignificant volume.
Vulvovaginitis, cervicitis, endometritis, salpingoophoritis - all these are inflammatory diseases of the internal and external genital organs, the manifestation of which is the presence of copious foul mucous discharge of yellow or green color.
Thrush is a fungal infection of the vagina that has striking symptoms, including a change in the nature of the discharge, the appearance of a milky-white color, consistency and smell of cottage cheese.
Venereal diseases. With these diseases, the nature of the woman’s discharge also changes: thick, viscous mucus, reminiscent of snot, turns into an abundant foaming liquid mass of gray color in case of chlamydia, heterogeneous, foul-smelling gray mucus with a yellow-green tint in case of gonorrhea, trichomoniasis, genital herpes, mycoplasmosis.
What is mucous discharge
The body is designed in such a way that mucus is released from the vagina at any phase of the menstrual cycle. This method maintains optimal vaginal microflora and removes harmful microorganisms, keratinized epithelial remnants, etc.
Mucous discharge after menstruation is colorless, not voluminous, and does not cause discomfort. Before ovulation, the number of clots increases.
A different situation occurs when the second half of the cycle begins. Before menstruation, clots may have a sour odor and a cheesy consistency. The volume becomes abundant and the hue becomes whitish. On underwear they turn yellow.
There are several indicators indicating normal discharge.
- the mucus has no odor, or it is faint, smells like fermented milk products;
- The color of the mucus is transparent or white, sometimes the color is white-yellow;
- The consistency of the leucorrhoea is thick, the clots are slightly stretchy, similar to snot.
Women do not feel any unpleasant symptoms (itching or burning). Usually one panty liner is enough to contain all the discharge.
Not all women know what leucorrhoea means and whether it is dangerous to health. In cases where they are accompanied by additional symptoms, it is recommended to consult a doctor.
How does vaginal discharge change during the cycle?
As already mentioned, cervical mucus changes its characteristics during the cycle due to hormonal influences and physiological changes. Qualitative and volumetric changes in discharge can indicate whether the menstrual cycle is normal.
Main changes:
- Immediately after your period, a minimal amount of cervical mucus is produced. Some women complain of excessive dryness during this time. However, the nature of the mucus may change over time: the fluid may become white, green or yellowish.
- Just before your period, estrogen levels begin to rise sharply, causing the cervix to produce more mucus. Sometimes the mucus at this time is compared to egg white. At this time, clear, odorless discharge appears. This liquid is an ideal protective environment for sperm. The most fruitful days of the cycle are characterized by maximum volumes of fluid.
- During ovulation, vaginal discharge becomes very intense. During this period, the consistency of the mucus may change - it becomes thick and resembles snot. These days are the most productive for fertilization.
- Discharge after ovulation is less mucus-like. There may be a change in the color of the discharge.
The vaginal discharge itself, like snot, can be observed during and after ovulation.
It is important to note that these phenomena are not the same for all women. The individual characteristics of the secreted fluid do not necessarily indicate possible diseases - this may be due to the patient’s anatomy or hormonal levels.
Why do they stand out?
Natural reasons that influence the appearance of leucorrhoea include:
- fluctuations in estrogen and progesterone levels during the menstrual cycle;
- hormonal changes - during menopause, during adolescence;
- use of oral contraceptives;
- stressful situations;
- period of sexual arousal;
- allergic reaction to underwear, condoms, etc.;
- insufficient or improper hygiene of the genital organs.
Dangerous causes of clots: sexually transmitted diseases or inflammatory infections of the genitourinary system. Often pathologies accompany each other. Any disease lowers immunity and opens up the possibility of developing other diseases.
Hormonal reasons
During pregnancy, hormonal levels change, which leads to an increase in leucorrhoea. If they do not cause discomfort, then this is a normal reaction of the body. By the second trimester, the mucus becomes less watery.
After childbirth, the clots increase in volume, become transparent, and stretch like snot. They have no smell, and the color can be not only transparent, but also yellowish.
If mucus with blood is observed while carrying a baby, this indicates a threat of miscarriage.
Female reproductive organs and ovulation
The main reproductive organs of a woman include the ovaries, uterus, oviducts and vagina. This is a system of interconnected anatomical structures, the main purpose of which is to ensure fertilization, pregnancy and further childbirth.
Ovulation is necessary for fertilization and subsequent pregnancy. Ovulation is the release of a mature female reproductive cell from the ovaries, occurring in the middle of the cycle. The egg enters the oviduct, where a favorable environment has already been created for fusion with the male reproductive cell. All these mechanisms require the active influence of female sex hormones. Changes in the characteristics of vaginal mucus are also associated with the listed phenomena.
During the menstrual cycle, the tissue of the uterus changes - a thicker outer layer is formed, which is necessary for the subsequent implantation of the embryo. If fertilization does not occur, then before a new cycle the uterus gets rid of functional tissue. The process of getting rid of tissue is accompanied by bleeding and characteristic vaginal discharge. It is during this period that discharge in the form of snot with bloody clots may appear.
In mature women, sooner or later the so-called menopause occurs. During menopause, ovulation and menstruation stop. This period is also not characterized by the appearance of vaginal secretions. Mucous or liquid discharge indicates an abnormality of menopause.
Knowledge of female reproductive physiology is important for assessing vaginal discharge.
When it comes to illness
If an inflammatory process is observed in the female body, then the color and aroma of leucorrhoea also change.
The main dangerous symptoms include:
- yellow, green or gray mucus clots;
- the pungent odor of the secreted substance - it can be putrefactive, similar to rotten fish or sour milk;
- copious amounts of watery leucorrhoea, stretching like snot;
- with streaks of blood in clear discharge (not related to menstruation).
In gynecology, it is customary to identify a number of diseases where lingering discharge plays the role of a key symptom.
Among them are the following:
- Chlamydia is a sexually transmitted infection that produces a huge amount of mucus that looks like snot. They are transparent or whitish in color;
- thrush is a fungal disease characterized by thick leucorrhoea. When examined, they look like white cottage cheese with a characteristic pungent and sour odor;
- genital herpes is a viral infection in which odorless mucous discharge and a rash on the genitals are observed;
- Trichomoniasis is a venereal disease that produces a lot of foamy mucus clots. They are characterized by a pronounced yellow or green tint, this indicates a purulent process;
- gardnerellosis - profuse leucorrhoea is accompanied by a strong smell of rotten fish;
- Gonorrhea is a sexually transmitted infection in which there is mucus (yellow or greenish) mixed with pus.
Voluminous, snot-like leucorrhoea is also diagnosed during diseases in which the genital organs (labia majora or minora) become inflamed. Pathologies include cervicitis, vulvovaginitis, endometriosis, etc.
What is considered normal
There are a number of cases when female discharge is a natural reaction of the body to external factors.
These are the following situations:
- After sexual intercourse without barrier methods of contraception, whitish clots are noticeable. This is a normal situation, it will stop after 2 - 4 hours;
- White mucous discharge in women, which is similar in consistency to cream, is observed after sex using condoms.
Often women take hormonal birth control pills. In these situations, they may experience brownish discharge (streaked with blood).
But if there are additional symptoms (unpleasant odors or pain in the perineum), then it is recommended to go to an appointment and get checked by a doctor. This condition is diagnosed with endometriosis or chronic endometritis.
When to go to the doctor
Women's health is an important component of a fulfilling married life. If discomfort or other unpleasant symptoms occur, you should consult a doctor.
Warning signs include:
- pain localized in the lower abdomen;
- changes in the menstrual cycle (mucous periods);
- pain when emptying the bladder and sexual intercourse;
- elevated temperature, but no other signs of acute respiratory viral infection, general malaise;
- itching, burning sensation or rash on the labia and vulva;
- swelling and hyperemia of the vaginal mucosa.
Preventive actions
A number of infections can be prevented by following simple rules. With regular adherence, the risk of clots is significantly reduced.
Preventive measures include:
- when having sex with casual partners, be sure to use barrier methods of contraception;
- After unprotected sexual intercourse, wash yourself thoroughly;
- wear only cotton or linen underwear, synthetics irritate the labia. It is also not recommended to wear tight panties;
- If any infections of the genitourinary system occur, immediately contact a gynecologist and undergo treatment. Advanced diseases aggravate women's health and can lead to difficulties in conceiving a child or to infertility;
- Maintain personal hygiene, wash your intimate organs daily, avoid aggressive care products (they are harmful to beneficial microflora).
Conclusion
Heavy mucous discharge can be caused by various reasons. Sometimes this is the body's reaction to external factors. In these cases they are safe for health.
Doctors warn! Shocking statistics - it has been established that more than 74% of skin diseases are a sign of parasite infection (Accarida, Giardia, Toxocara). Worms cause enormous harm to the body, and the first to suffer is our immune system, which should protect the body from various diseases. The head of the Institute of Parasitology shared the secret of how to quickly get rid of them and cleanse your skin, it turns out that’s enough. Read more .
When leucorrhoea is accompanied by other signs (pain, pain when urinating, unpleasant odor), this indicates problems in the functioning of the genitourinary system; for diagnosis it is worth going to a gynecologist. He will explain what it means and tell you how to treat it.
«>
Memo for postpartum women upon early discharge from the hospital
Since contraction of the uterus occurs due to the work of muscles, this is accompanied by pain of varying intensity, reminiscent of mild contractions. You may notice increased pain while breastfeeding your baby. The thing is that stimulation of the nipple causes an increase in the level of oxytocin in the blood, which promotes uterine contractions. For better contraction of the uterus, it is recommended to lie on your stomach after childbirth. If you feel good, try to move more and do gymnastics. Another worrying circumstance is pain in the perineum, which appears even if there were no tears and the doctor did not make an incision.
This occurs because the tissues were subjected to severe stretching during childbirth. Usually the pain is not very intense and goes away within a day. But if there were tears or an incision in the perineum, then the pain may last longer—days. You should carefully monitor the stitches and perform hygiene after each visit to the toilet.
In addition, it is necessary to treat the stitches daily with antiseptic solutions, and you cannot sit for 2 weeks.
After childbirth, hemorrhoids often appear. Good hygiene and a daily evening shower can help reduce pain. Don’t forget about your diet, include in your diet foods that are rich in fiber and have a mild laxative effect: seaweed, beets, baked apples, cauliflower, sprouted grains. Medicines are usually not used because the inflammation goes away in most cases over time. If everything does not go away on its own and the woman continues to suffer from hemorrhoids, you need to see a doctor and use the medications prescribed by him or take a course of physiotherapeutic procedures.
Constipation that occurred during pregnancy may continue to recur in the postpartum period. They are, in particular, caused by the fear of damaging the seams on the perineum.
However, such fear is in vain. In addition, during defecation, you can hold the area where the stitches are placed with a napkin, which will reduce tissue stretching, and defecation will be less painful. Stool usually does not occur immediately after childbirth, but every other day. To prevent constipation, eat prunes and dried apricots, drink mineral water. And only if there was no bowel movement on the 3rd day, you can use a laxative suppository. After childbirth, particularly strong discharge from the uterus is observed in the first day, then it decreases.
After just 3 days, the discharge becomes mucous-bloody. By the 1st week after birth, discharge from the uterus stops altogether. During this period, you need to carefully observe hygiene, because an infection that gets into the uterus can lead to endometritis, an inflammatory process of the uterine mucosa. However, the functions of a woman-mother did not end there. The main one - providing the baby with food - is taken on by the mammary glands. Hormonal changes continue in a woman’s body, due to which significant changes occur in the mammary glands, and they begin to produce milk.
In the first days, colostrum is released, and already on the 1st day, transitional milk is released, which gradually turns into mature breast milk. Feeding your baby stimulates milk production. Therefore, if lactation is insufficient, more frequent breastfeeding is recommended. However, women often face the opposite problem - excess milk and difficult outflow.
This, in turn, leads to stagnation and engorgement of the mammary glands - they harden, increase in volume, and painful sensations appear in the breast area. Your body temperature may even rise. How to prevent such phenomena? First of all, try to breastfeed your baby regularly, and in the first days after birth, limit fluid intake to ml per day.
Then the mammary glands will gradually become soft again. In addition, it is important to know that in the first days after childbirth, the skin of the nipples is very delicate and may crack. This makes them vulnerable to infection, the entry of which into the cracks can lead to the development of mastopathy.
Therefore, you need to take good care of your nipples and wear a comfortable bra, which will help the proper development of lactation. To prevent cracks from appearing on the nipples, you need to alternately place the baby on each breast in the first days after birth. First, give the baby one for a minute, then the other for a minute. To prevent cracks, there is a special cream that should be used between feedings, and before them, thoroughly wash off its remains.
These are all the troubles that are easily forgotten and seem not so significant against the backdrop of new worries. Now your attention will be constantly occupied by the baby. However, it is very important not to forget about yourself, maintain your health and restore your former beauty.
Not everyone succeeds, which contributes to the development of postpartum depression. After childbirth, under the influence of cellular enzymes secreted by the granulation shaft, blood clots and fragments of the decidua remaining on the walls of the uterus are liquefied.
In addition, leukocytes, erythrocytes, plasma and lymph penetrate into the uterine cavity through the wound surface. All these elements form lochia - postpartum wound secretion, which normally actively flows from the uterine cavity through the cervical canal into the vagina.
The first days after birth, lochia is bloody in nature, then, from the first day, it acquires a dark red and brownish tint, and after a week it becomes yellowish-white due to the high content of leukocytes. From the 10th day, the discharge becomes light, watery, and has a serous-mucous consistency. Gradually, the amount of lochia decreases, and by the end of the 3rd week, the discharge practically stops and soon disappears completely.
When there is a delay in the outflow of postpartum secretions, they speak of a lochiometer - stagnation of lochia in the uterine cavity. The danger of developing lochiometra lies in the high probability of infection of the contents of the uterus, since lymph, serum, blood, and tissue debris serve as the best nutrient medium for the proliferation of microbial flora.
Most often, endometritis develops against the background of lochiometra. The development of lochiometra is caused by mechanical obstacles to the outflow of secretions in the cervical canal or insufficient contractility of the uterus.
Mechanical obstacles can be caused by kinks, hyperanteflexion of the uterus or blockage of the cervical canal by blood clots, remnants of the decidua and exfoliated uterine tissue. Insufficient contractile activity of the uterus in the postpartum period usually develops as a result of overstretching of the uterus with a large fetus, polyhydramnios or multiple pregnancies, weak or discoordinated labor.
Lochiometra develops one day after birth and is characterized by a noticeable decrease or cessation of postpartum discharge from the uterus. In this case, there is an increase in the size of the uterus compared to the norm on the current postpartum day, and its pain on palpation. The general health and objective condition of the woman during the lochiometer does not suffer, the body temperature is normal, there is no tachycardia. After 24 hours, the temperature drops critically with the simultaneous appearance of liquid, purulent lochial discharge.
Lochiometra is diagnosed based on characteristic clinical signs. With the help of a gynecological examination, an unevenly enlarged and painful uterus is determined, which has a dense elastic consistency, often - closure of the internal pharynx, and an inflection of the uterus. Clarifying diagnostics of lochiometers includes ultrasound. Treatment of lochiometra is to ensure the free outflow of lochia, taking into account the cause that caused this condition.
When lochiometra is detected, the gynecologist prescribes injections of the antispasmodics papaverine and no-shpa to relieve spasm of the uterine pharynx. In the treatment of lochiometra, uterotonic uterine contractions are used - oxytocin, methylergometrine. For free outflow of secretions, it is recommended that the postpartum woman lie on her stomach 2-3 times a day for 1-2 hours.
With hyperanteflexia of the uterus, the bend is eliminated during a bimanual examination; physical therapy is prescribed. In the case of lochiometra, caused by blockage of the cervical canal with clots, during examination on the chair, the cervical canal is manually expanded and the clots are carefully removed.
Clinical gynecology considers situations where lochiometra does not resolve within x days as an indication for instrumental removal of the contents of the uterus with a curette or vacuum apparatus under the control of hysteroscopy. For the prevention and treatment of postpartum infections due to lochiometra, antibiotics are prescribed taking into account the results of a bacteriological smear. If, after the elimination of lochiometra, uterine pain, poor contraction, and hyperthermia persist, one should think about the development of postpartum metroendometritis.
If the infection progresses, the condition of the postpartum mother may worsen due to the development of purulent-resorptive fever, manifested by intoxication, abdominal pain, purulent discharge with a putrid odor.
Against this background, the transition of lochiometra to pyometra is noted. To prevent the development of lochiometra, competent management of pregnancy and preparation of the woman for childbirth is required, as well as careful monitoring of the mother during the postpartum period: regular monitoring of uterine contractions, daily palpation determination of its sensitivity, consistency, fundal height, volume and nature of discharge.
In the postpartum period, a woman needs to monitor the timeliness of emptying the bladder and intestines, breastfeed the newborn upon request, perform postpartum exercises, and lie on her stomach.
After discharge from the maternity hospital, the young mother should also monitor her well-being and discharge from the genital tract. In case of fever, retention of lochia, changes in their character or smell, immediate contact with a gynecologist is necessary. The prognosis for timely detection and elimination of lochiometra is favorable. You must have JavaScript enabled to view it. Export of medical services 1gkb-bel. Home Information for citizens Doctors inform Recovery after childbirth.
Lochiometra After childbirth, under the influence of cellular enzymes secreted by the granulation shaft, blood clots and fragments of the decidua remaining on the walls of the uterus are liquefied. Reasons for the development of lochiometra The development of lochiometra is caused by mechanical obstacles to the outflow of secretions in the cervical canal or insufficient contractility of the uterus.
The development of lochiometra is facilitated by prolonged bed rest and low activity after childbirth. Symptoms of lochiometra Lochiometra develops one day after birth and is characterized by a noticeable decrease or cessation of postpartum discharge from the uterus. Diagnosis of lochiometers Lochiometers are diagnosed based on characteristic clinical signs.
Treatment of lochiometra Treatment of lochiometra is to ensure the free outflow of lochia, taking into account the cause that caused this condition. Complications of lochiometra If, after the elimination of lochiometra, uterine pain, poor contraction, and hyperthermia persist, one should think about the development of postpartum metroendometritis.
Prevention and prognosis with lochiometra To prevent the development of lochiometra, competent management of pregnancy and preparation of the woman for childbirth is required, as well as careful monitoring of the mother during the postpartum period: regular monitoring of uterine contractions, daily palpation determination of its sensitivity, consistency, fundal height, volume and character discharge. Minsk, Nezavisimosti Ave., Security measures.
Development and support of the gt-systems website.