Menstrual irregularities, development of adhesions, chronic posthemorrhagic anemia and even infertility. All these are consequences of endometriosis. According to medical statistics, endometriosis is one of the most common gynecological pathologies. It ranks third in terms of the number of requests, behind only uterine fibroids and inflammatory diseases of the reproductive system. The development of this pathology can be triggered by a malfunction of the immune system, hormonal imbalance, complicated childbirth, or even simple overwork.
Both conservative and surgical therapy are used to treat endometriosis. The most effective method of treating this pathology is endoscopic coagulation of endometriotic lesions.
If you are thinking about surgical treatment of endometriosis, you should give preference to a multidisciplinary medical center that provides a full range of services in this area.
The Center for Obstetrics and Gynecology ON CLINIC is equipped with the latest endoscopic equipment of an expert level, which allows us to carry out the full range of gynecological operations, achieving maximum treatment results. Endoscopic coagulation of foci of endometriosis is a rather complex operation that can only be performed efficiently by a doctor with sufficient experience in performing such interventions. These are the specialists who work at ON CLINIC.
Coagulation of endometriosis foci
Coagulation of endometriosis foci can be carried out in the initial stage of this disease. It represents the growth of endometrial-like tissue outside the uterine cavity (only here it should be normal). Atypically located endometrium also has a menstrual-like function. Endometriosis can affect various organs, both genital and extragenital. The danger of this disease is as follows:
- Violation of reproductive function in the form of infertility
- Persistent pain syndrome
- Development of the adhesive process between the pelvic organs.
Indications
Coagulation of endometriosis foci is carried out in the following cases:
- Cervical lesions
- Intraoperatively detected lesions on the pelvic organs are small in size.
Most often, the operation is performed for infertility, and after coagulation of endometriotic lesions and appropriate conservative treatment, reproductive function is usually restored.
General characteristics of the procedure
Coagulation of endometriosis foci is performed after pain relief. An electrode is applied to the endometriotic areas and an electric current is applied. This causes the death of pathological cells. However, to prevent relapse of the disease, it is necessary to carry out complex conservative therapy, which is aimed at the systemic causes of this pathological process.
Contraindications
Contraindications for coagulation of endometriotic lesions are:
- Exacerbation of the inflammatory process in the organs of the reproductive system
- Common form of the disease
- Endometrioid ovarian cysts, when there is no technical possibility of coagulation.
Possible complications
Complications of electrocoagulation of endometrioid lesions are:
These complications are not common compared to traditional surgical excision, so electrical coagulation is preferred when conditions and indications exist.
In conclusion, it should be noted that coagulation of endometriosis foci is a local treatment for this disease. However, it can only be carried out with a certain localization of pathological foci. In combination with conservative therapy, coagulation allows one to achieve a good therapeutic result and restore reproductive function, as well as cope with chronic pelvic pain syndrome.
Share with your friends:
Key news tags:
Other news on the topic:
- Pharmacy presents: Rebetol (Ribaverin)
- Possible complications after an abortion
- Cervical erosion during pregnancy: dangerous or not?
- Tonsillitis in children
- Frozen pregnancy. Causes
- Male infertility. Causes and treatment
P rendering
The main indication for treatment is focal endometriosis. The lack of effectiveness of drug therapy becomes the reason for prescribing coagulation. If a woman has no signs of a pathological process, doctors may postpone the operation for a while and try to cope with the disease with the help of potent hormones.
Coagulation of endometriosis is prescribed to women with the following complaints:
- frequent spontaneous uterine bleeding;
- chronic pelvic pain;
- infertility;
- prolonged menstruation, accompanied by brown spotting;
- adhesive process;
- ovarian dysfunction;
- history of ectopic pregnancy, the cause of which was damage to the fallopian tubes.
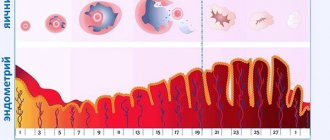
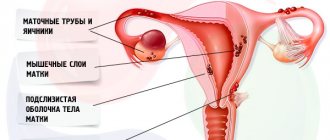
Characteristics of the disease
To understand the essence of the disease, you need to understand the mechanism of its occurrence. The inner layer of the uterus is represented by the endometrial layer. If there are no pathological processes, then the upper part of the endometrial layer is separated during menstruation and, together with the blood, comes out through the vagina. If pathological changes are observed in the female body, endometrial elements penetrate the internal organs and settle on their walls, which should not normally happen.
The endometrial layer can be transported through the bloodstream to the fallopian tubes, female reproductive glands and other organs. Here these cells settle, begin to grow, and on the days of menstruation they begin to bleed, but the blood does not find a way out. This leads to compression of the nerve endings, which provokes severe pain, and often leads to an adhesive process, which is the cause of infertility.
Symptoms of endometriosis:
- pain a few days before and during menstruation (the more advanced the disease, the longer the pain persists during menstruation);
- pain during menstruation is directed from the abdomen to the lumbar region and tailbone;
- intense bleeding during menstruation;
- bleeding from the uterus not associated with the menstrual cycle;
- menstrual irregularities;
- problems with conception.
Depending on the site of implantation of endometrial elements, specific signs may appear:
- pain when passing stool if the endometrial layer grows into the wall of the rectum;
- pain during urination if germination occurs in the bladder;
- pain during sexual intercourse with damage to the cervix and vagina.
If endometriosis is not treated at the first symptoms, additional unpleasant consequences develop:
- changes in the nervous system: irritability, tearfulness, sudden mood swings;
- frequent headaches, dizziness and nausea of unknown etiology;
- pain in the pelvic organs;
- increase in body temperature.
Risk factors for developing endometriosis include:
- shortened menstrual cycle,
- heavy menstrual flow with blood clots,
- obesity,
- use of an intrauterine device,
- age from 30 to 45 years,
- high concentration of estrogen in the blood,
- hereditary predisposition to endometriosis.
Preparation
In order for the intervention to be as effective as possible and for the patient to tolerate it easily, you need to undergo a little preparation. Namely:
- Do not drink alcohol at least two days before the intervention, and do not drink it for three to four days after it;
- After consulting with your doctor, stop taking blood thinning medications at least a week before the intervention (if possible, if there are no vital indications for taking them);
- Conducting studies (ultrasound, MRI, colposcopy, etc.) and tests (for hormones, blood clotting, etc.);
- Five days before the intervention, you must start drinking activated carbon;
- Four days before surgery, stop eating foods that cause bloating or gas;
- On the eve of the operation, an enema is given, and sometimes gastric lavage is also done;
- A few hours before the operation, you need to take a shower and remove hair on the stomach and groin area.
If all these details are followed, the operation will be easy and the recovery period will be short.
Treatment of endometriosis
An effective way to get rid of endometriosis is considered to be laser removal of the pathological focus, which is complemented by hormonal replacement therapy.
The Clinic widely uses radio wave coagulation of endometriosis lesions. The operation is performed using the Surgitron apparatus. This device is a kind of generator of high-frequency electric waves that are emitted in the area of the pathological focus. As a result, “abnormal” cellular elements “evaporate” and the walls of the operating area coagulate. In this case, the blood vessels are sealed, which prevents the development of postoperative bleeding.
The advantages of the radio wave method over others are:
- painlessness,
- no postoperative complications,
- quick recovery period after surgery.
This is due to the fact that the tissues surrounding the surgical area are not damaged. And in the incision area, the tissues are cauterized, which leads to an antiseptic effect and rapid healing in the future.
Cost of services
The cost of coagulation depends on the following factors:
- clinic providing the service (in public medical institutions the operation is performed free of charge if you have insurance);
- the region in which the manipulation is carried out;
- localization of foci of endometriosis (in the vagina or abdominal cavity);
- stages of the pathological process;
- coagulation method (laser exposure, nitrogen treatment or cauterization);
- qualifications of the specialist providing the service;
- further observation and control during the rehabilitation period.
In private medical institutions specializing in the treatment of endometriosis, the cost of the operation starts from 40-50 thousand rubles.
Endocoagulation of endometrioid heterotopias
Endocoagulation - a method of thermal destruction of foci of endometriosis is used as an independent method of treatment of external genital endometriosis or as a stage in combination with hormonal treatment: combined estrogen-gestagen drugs, progestogens, antigonadotropic drugs.
The safest and most gentle method of thermal destruction of endometrioid heterotopias is endocoagulation according to the Zemm method, carried out at a temperature of 90-100°C.
Endocoagulation of foci of endometriosis should begin after a thorough examination of the entire accessible surface of the pelvic organs and parietal peritoneum, identification and fixation of all visible foci of endometriosis and all suspicious areas, and determination of the degree of spread of endometriosis.
The optimal days of the menstrual cycle for endoscopic diagnosis of external genital endometriosis are the late luteal phase and the first days after the end of menstruation.
When performing laparoscopy on other days of the menstrual cycle, when foci of endometriosis are not so clearly visible, as well as in doubtful cases, it is recommended to perform the so-called “thermo-color test”. The working end of the endocoagulator, heated to 100°C, is slowly passed over suspicious areas. In this case, the healthy peritoneum becomes white due to the burn, and endometriotic heterotopias become brown or black due to the content of hemosiderin and other hemoglobin breakdown products. Fresh hemorrhages remain red, only the intensity of the color changes. Before starting the endocoagulation procedure, it is necessary to clarify the depth of the lesion, to what extent the foci of endometrioid growths located on the parietal peritoneum and the peritoneum covering the bottom of the bladder and other organs are fused with the underlying tissues, especially in areas of projection of large vessels and ureters. To do this, using Zemm biopsy forceps or atraumatic forceps, grasp the fold of the peritoneum next to the affected area and, lifting it, move it in different directions. When the underlying tissues grow, the affected areas hardly move relative to the subperitoneal tissue and rise along with it.
If endometriosis grows into the ureteral wall, endocoagulation of these areas should not be performed.
You should also refrain from coagulating foci of endometriosis located on the intestinal wall, since endometriotic growths of this localization, as a rule, grow into the muscular layer of the intestinal wall very early.
It must be remembered that a biopsy of endometriosis foci for the purpose of histological confirmation of the diagnosis should be performed only in doubtful cases, since it has been established that the visual endoscopic picture is sufficient to make a diagnosis of external genital endometriosis.
A biopsy of foci of external genital endometriosis is performed using two instruments as follows:
Using atraumatic forceps or Zemm biopsy forceps, they grasp the peritoneum in the immediate vicinity of the lesion and lift it so that a fold of the peritoneum is formed. At the top of the fold there will be a scar with endometriotic growths. Frankenheim biopsy forceps inserted through the second surgical trocar are used to grasp the top of the peritoneal fold containing the endometriosis lesion in such a way as to capture all layers of the endometrioid formation and bite it off. The edges of the resulting peritoneal defect are carefully coagulated with a point coagulator at a temperature of 100-120° C in order to destroy the remaining endometrioid tissue.
In order to destroy all visible endometriotic lesions, endocoagulation of endometriosis foci is performed sequentially in all areas of the peritoneum, moving from one area of the pelvis to another, starting from the anterior uterine space, clockwise. It is best to carry out destruction using a point endocoagulator. Coagulation is carried out by firmly touching the lesion with the coagulator turned on. Slowly stroking the working part of the endocoagulator, coagulate the affected surface over the entire area of the heterotopia and retreating 2-3 mm beyond it. It should be remembered that at a temperature of 100-120°C, tissue coagulation occurs to a depth of approximately 1 mm within 10 seconds. Endometriotic lesions of the uterosacral ligaments often penetrate into the tissue to a considerable depth. Taking this into account, it is necessary to perform endocoagulation of the growths to their entire depth. If it is impossible for the end of the point endocoagulator to penetrate deep into the lesion, the surface layer can be cut with scissors.
Methodology
Depending on the location of the foci of endometriosis, vaginal or laparoscopic coagulation is performed. For lesions located on the mucous membrane of the external genitalia or the cervix, cauterization is performed under local anesthesia. This method is rarely used, since this form of endometriosis is not common.
Coagulation using laparoscopy is performed according to the following algorithm:
- the patient is given anesthesia;
- the anterior abdominal wall is lifted by introducing gas;
- the stomach is pierced in several areas;
- instruments and a coagulation device are inserted through trocars (special tubes);
- the pathological area is grabbed with forceps and treated with a beam, electric current or frozen at low temperatures;
- foci of endometriosis are removed one by one;
- analyze the condition of the pelvic organs - determine the patency of the tubes, examine their ovaries on one side and the other, the abdominal cavity and intestines;
- toilet the abdominal cavity and remove instruments;
- the holes are sutured or sealed with a plaster.
Types of operations
Surgery involves excision or coagulation of abnormal lesions. Common methods of treating the disease include:
- laparoscopy – a minimally invasive form of surgery;
- laparotomy - penetration through the peritoneum to the internal organs;
- through vaginal access.
Surgery to eliminate foci of endometriosis on the pelvic peritoneum
Therapy includes the following stages:
- full diagnostic examination of the problem area;
- determination of volumes and areas of pathological foci;
- preliminary preparation for removal of overgrown tissue - dissection of formed adhesions and other procedures;
- cauterization or removal of problem areas using electric currents, a laser beam or thermal effects.
Surgical treatment of ovarian endometriosis
Surgical removal of endometriosis includes a step-by-step algorithm:
- the problematic ovary is isolated from adhesions, which are cut using a surgical instrument;
- the doctor performs a resection along the boundaries of the unaffected tissue, the body of the focus of pathological activity is excised;
- the location of the lesion is treated with a laser beam or electrodes in order to restore hemostasis;
- internal organs located in the abdominal cavity are washed.
The body of the cyst is sent for histological examination. Removal of the entire pathology is possible if its size does not exceed 3 cm in diameter. Larger tumors are removed in parts.
Surgical treatment of retrocervical endometriosis
In clinics, preference is given to the laparovaginal technique. Excision of the endometriosis lesion occurs through vaginal access, at the same time a laparotomy is performed to control the removal process and assess the severity of the pathological process. At the end of the manipulation, the intervention area is treated with laser or electrode technology.
Laparoscopic surgery
It is a minimally invasive method of surgical intervention with minimal damage when accessing the uterus. Three minimal incisions are made on the anterior wall of the peritoneum through which surgical instruments are inserted.
Full control over the procedure and minor damage during the operation make it possible to preserve the patient’s reproductive function and stop further progression of the disease.
Scraping
Includes two solutions to the problem:
- separate entry - during the operation, the cervix is initially cleaned, followed by the cavity;
- traditional - involves removing all tumors blindly, which often contributes to damage and the development of complications.
The resulting material undergoes histological examination.
Contraindications
The list of contraindications for surgical intervention is long. Before the procedure, it is necessary to examine the body and exclude the following conditions:
- infectious and inflammatory diseases in acute form;
- a decrease in platelets, causing a deterioration in blood clotting;
- surgical interventions performed less than 3 months ago;
- type diabetes;
- vascular pathologies, tendency to form blood clots;
- disruption of myocardial function (uneven heartbeat, surges in blood pressure);
- infections of the lower and upper respiratory system;
- skin diseases localized in areas of access to foci of endometriosis;
- obesity or overweight with a large layer of fat in the peritoneal area;
- allergic reactions to medications used during surgery;
- disease of filter organs (liver, kidneys);
- malignant neoplasms;
- inflammation of the abdominal cavity;
- pregnancy of any stage or suspicion of it;
- breastfeeding (due to anesthesia).
Removal of the uterus and consequences
Excision of the affected organ in case of endometriosis occurs in several ways: radical or laparoscopic. After the intervention, the patient is observed in the hospital. With laparoscopy, discharge takes 3-5 days; with classical surgery, the woman is delayed for two weeks until the suture material is removed.
After the surgical procedure, complications may develop:
- inflammatory and purulent processes in the suture area;
- peritonitis;
- impaired urination;
- pulmonary thromboembolism;
- internal or vaginal bleeding.
To prevent consequences, you must follow your doctor's advice and wear a special bandage to support the abdominal muscles. For two months, a woman should not use tampons, take hot baths, or visit steam rooms, baths and saunas.
Contraindications
In what cases is this type of intervention contraindicated? There are a number of general contraindications to laparoscopy. Since this method is used in coagulation, these should also be taken into account. This:
- Poor blood clotting;
- Inflammatory and infectious processes in the body;
- Recent pelvic surgery;
- Tendency to form scars and adhesions;
- Diabetes;
- Diseases of the cardiovascular system;
- Respiratory diseases;
- The presence of skin diseases or scars on it in the puncture area;
- Obesity due to inability to access;
- Intolerance to anesthesia;
- Depression of liver and kidney functions, etc.;
- Exacerbation of chronic diseases;
- Tumors of any etiology, including unclear and benign;
- Peritonitis of the abdominal cavity;
- Pregnancy, last trimester;
- Cerebrovascular accident.
Life after the procedure
Before discharge from the medical institution, the patient is explained in detail the rules:
- for the first two months, any physical activity and sexual intercourse should be excluded;
- transition to a balanced daily menu enriched with plant fiber;
- excluding the use of alcohol, low-alcohol products, and narcotic substances;
- sports training according to the strength and capabilities of the body;
- daily walks in the fresh air;
- compliance with intimate hygiene requirements;
- refusal to use intrauterine contraceptives - spirals.
Methodology
The operation is performed in the same way as any other laparoscopy. This is done in several stages:
- The patient is put under anesthesia;
- Carbon dioxide is injected into the peritoneum;
- Using a laparoscope, the abdominal wall is pierced in the navel area or just below it and a camera is thus inserted into the uterine cavity;
- Then two more punctures are made, on both sides of the abdomen, through which instruments for carrying out the intervention are inserted (a loop, an applicator with liquid nitrogen, or something else);
- Using camera readings, the doctor visually assesses the amount of work and then performs cauterization (the most popular and simple method is Zemm coagulation);
- A metal loop is inserted into the uterine cavity, the working end of which is heated to a temperature of 60-90 degrees using an electric current;
- The location of the affected areas is determined;
- They are grabbed one by one with special forceps and cauterized;
- Exposure lasting 10 seconds allows you to evaporate the area to a depth of about 1 mm;
- If the areas are too deep, then cauterization is also supplemented with excision or curettage;
- If necessary, some vessels are ligated;
- The instruments are removed;
- No stitches are required.
Visualization of foci of adenomyosis is best done in the first phase of the menstrual cycle. But the intervention can be carried out at another period. But if the doctor has doubts about where the healthy tissue is and where it is overgrown, then he conducts a thermocolor test. This is a manipulation in which, under the influence of high temperatures, healthy tissues become light white, and damaged tissues become brown or black.
Appearance of lesions
Recently, the use of the Zemm electrocoagulation method has increasingly been abandoned in favor of the use of laser surgery methods. It is believed that laser treatment, with the same effectiveness, is less dangerous and traumatic.
Treatment of endometriosis using laparoscopy
Endometriosis is the 3rd most common pathology among all gynecological diseases. The development of the disease occurs due to the fact that cells identical to the inner layer of the uterus - the endometrium, begin to invade and function on other organs and tissues outside the uterus, leading to dysfunction of these organs and tissues. This happens for a number of reasons; there are several theories about the occurrence of the disease. The most common is the return of menstrual blood into the abdominal cavity through the fallopian tubes. Menstrual blood normally exits through the genital tract during menstruation, but it also happens that this blood ends up in the fallopian tubes and then enters the abdominal cavity. In this case, endometrial cells grow into the organs and tissues of the pelvis: the peritoneum, ovaries, sacrouterine ligaments, intestines, ureters and many others. Endometriosis can directly affect the uterine body itself, a condition called adenomyosis.
It is very important to note that with endometriosis, the main complaint is pain . The pain can be normal, during sexual intercourse, during menstruation, or radiate to the lower back or anus. Normally, a woman should not take painkillers during her period. If this happens constantly, then there is a high probability of endometriosis. Menstruation with endometriosis is not only painful, but also often heavy, and there may be spotting from the genital tract before menstruation. Endometriosis can be a leading cause of infertility.
Diagnosis of endometriosis – the patient’s complaints about the disease correctly collected by the doctor, a mandatory gynecological examination, laboratory data – a blood test for the carbohydrate antigen CA-125, special instrumental research methods for organ dysfunction: ultrasound or MRI of the pelvic organs or uterus and appendages for endometrioid ovarian cysts , colonoscopy for endometriosis of the large intestine, excretory urography and cystoscopy for endometriosis of the genitourinary system. Adenomyosis or endometriosis of the uterine body can be detected using hysteroscopy - an endoscopic research method in which an optical instrument, a hysteroscope, is inserted into the uterine cavity through the vagina and cervix, to which a video camera with a monitor is connected. In this case, the surgeon immediately sees on the monitor the so-called endometrioid tracts in the uterine cavity, confirming the diagnosis of adenomyosis. Basically, instrumental research methods are limited to ultrasound diagnostics. In all textbooks, laparoscopy is called the “gold standard” for diagnosing endometriosis. This is true, but it is important to note the fact that laparoscopy for endometriosis is not just a diagnostic method, but in the right hands it is the best way to combat it.
Endometriosis is a surgical disease , that is, to achieve the goal of recovery, it is necessary to remove endometriotic lesions. In this case, the organ or tissue is freed from the affected area and restores its function. Foci of endometriosis cause changes in tissues or organs like scar tissue: they pull on themselves and change the normal structure of the underlying tissues, this can be called in one term - stricture. It is very important to clarify with the future surgeon how he plans to influence such foci or infiltrates of endometriosis. Exclusively “cauterization” or coagulation in this case is a very mediocre operation, which has a high risk of recurrence in an even worse form: such coagulation can enhance the effect of tissue stricture, which will further unite foci of endometriosis into an endometrioid infiltrate, and treatment of this kind is This is already an extremely complex and different level of operation. I repeat, foci of endometriosis should be removed as much as possible: pathological formations should be excised or resected to healthy tissue. This is the cornerstone of the surgical intervention. There are many medications available from the pharmaceutical industry to treat endometriosis. These drugs can stop the spread of cells at some initial level, but they will not remove the formed focus or infiltrate of endometriosis - this is only possible through surgery. A modern and correct approach to treatment is: first and foremost, surgery to remove foci of endometriosis and subsequent hormonal therapy for 6 months.
Preparation
Preparatory activities involve performing hardware, instrumental and laboratory diagnostics. A preliminary diagnosis can be made based on the patient’s complaints. Pathology can be confirmed by sonological examination (ultrasound).
On ultrasound, endometriosis is often mistaken for myomatous nodes, dermoid cysts and other pathologies. The most reliable diagnostic method is considered to be laparoscopy (for external endometriosis) and hysteroscopy (for the internal form).
If the patient has no contraindications for coagulation, preparation is prescribed:
- stop drinking alcohol several days before surgery, as alcohol thins the blood and can cause complications;
- Avoid taking medications unless prescribed by a doctor, especially aspirin and NSAIDs;
- 4-6 days before coagulation, start taking sorbents and carminatives in order to cleanse the intestines and prevent gas formation, which may interfere with the visualization of lesions;
- for 3 days, remove from the diet foods that provoke flatulence (fresh vegetables and fruits, legumes, baked goods, sweets);
- on the eve of the operation, refuse dinner and do not drink water after midnight;
- On the day of the procedure, a cleansing enema is performed, the consumption of water and food is excluded.
Immediately before coagulation, premedication is performed (preparation for the procedure with the help of medications). The woman is given injections of an antispasmodic, a sedative, and drugs that reduce the activity of the endocrine glands.